When you pick up a prescription, you might not think twice about whether it’s the brand-name drug or the cheaper generic version. After all, the FDA says they’re the same. But for some people, switching from a brand-name drug to a generic isn’t just a cost-saving change-it’s a health risk. Why do some patients feel worse after the switch? And why do others never notice a difference? The answer isn’t simple, and it’s not just about price.
The Myth of Perfect Equivalence
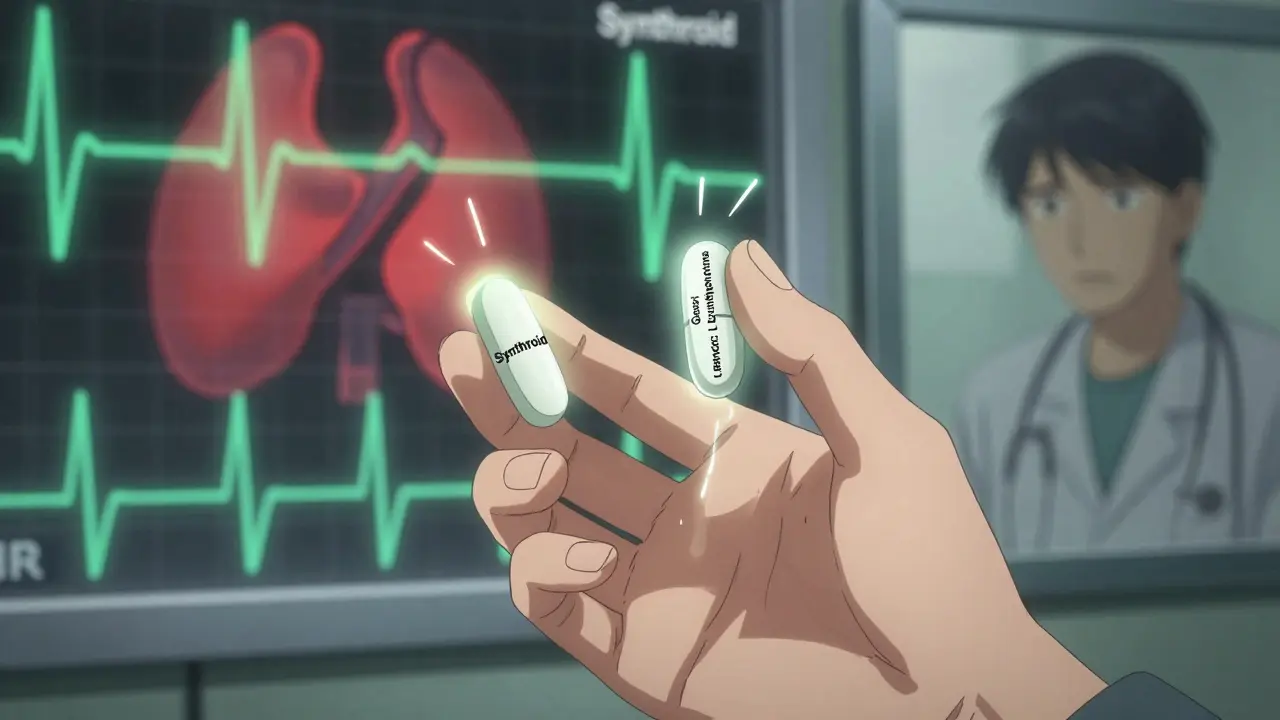
Generic drugs are required by law to contain the same active ingredient, dose, and route of delivery as their brand-name counterparts. That part is true. But what the FDA doesn’t tell you is that generics can differ in everything else-fillers, dyes, coatings, binders, and preservatives. These are called inactive ingredients, and they make up 80% to 99% of a pill’s weight. For most people, that doesn’t matter. But for others, it changes everything.Take levothyroxine, the most commonly prescribed thyroid medication. Brand-name Synthroid and its generics have identical amounts of levothyroxine sodium. But the way the body absorbs it can vary. A 2019 study in JAMA Internal Medicine found that nearly 24% of patients who switched from Synthroid to a generic version saw their thyroid hormone levels swing out of the safe range within six months. That’s not a small fluctuation-it’s enough to cause fatigue, weight gain, heart palpitations, or even a heart attack in vulnerable patients.
Narrow Therapeutic Index: When Small Changes Matter
Some drugs live on a razor’s edge. These are called narrow therapeutic index (NTI) medications. For these, the difference between a therapeutic dose and a toxic one is tiny-often less than double. A 10% change in blood concentration can mean the difference between control and crisis.NTI drugs include:
- Levothyroxine (for hypothyroidism)
- Warfarin (a blood thinner)
- Phenytoin and carbamazepine (for seizures)
- Digoxin (for heart rhythm)
The FDA allows generics to be 80% to 125% as bioavailable as the brand-name drug. That means two different generics of the same drug can differ by up to 45% in how much gets into your bloodstream-and still both be considered "bioequivalent." One generic might release the drug slowly. Another might dissolve too fast. For someone on warfarin, that could mean a dangerous spike in INR levels and risk of bleeding. For someone on phenytoin, it could trigger a seizure.
Real Patients, Real Reactions
Patient stories don’t always show up in clinical trials. But they tell the truth.On Drugs.com, 38% of people taking generic levothyroxine reported worse symptoms than when they were on Synthroid. Many described sudden fatigue, brain fog, and mood swings. On Reddit’s r/pharmacy, users consistently report problems with generic bupropion (used for depression and smoking cessation). One user wrote: "I switched to the generic and had headaches so bad I couldn’t work for three days. My anxiety spiked. My doctor said it was all in my head. Then I switched back-and I felt like myself again."
A 2022 survey of 3,215 U.S. pharmacists found that nearly 70% had seen patients react badly after switching between different generic brands of the same drug. Over 40% said this happened more than five times a month. These aren’t rare cases. They’re routine.
Why the System Allows This
The FDA’s approach is built on efficiency. The Hatch-Waxman Act of 1984 was designed to get cheap drugs to market fast. Requiring full clinical trials for every generic would delay access and raise costs. So instead, they rely on bioequivalence studies-usually done on 24 to 36 healthy volunteers. These studies measure average blood levels, not individual responses.But here’s the problem: healthy volunteers aren’t the people who take these drugs. A 72-year-old with kidney disease, a 28-year-old with a genetic variation in liver enzymes, or someone with celiac disease absorbing drugs differently-they’re not in those trials. And yet, they’re the ones getting switched to generics.
The FDA admits there are gaps. In 2023, they released draft guidance identifying 17 drug classes where generic substitution has caused documented problems. They’ve also approved the first "authorized generic" of Synthroid-made by the same company as the brand, just sold under a different label. It’s not cheaper than other generics, but it’s chemically identical. For patients who’ve had bad reactions, it’s a lifeline.
What You Can Do
If you’re on a medication with a narrow therapeutic index, don’t assume all generics are equal. Here’s what works:- Ask your doctor to write "Do Not Substitute" on your prescription. This stops the pharmacy from switching you without approval.
- Stick with one generic manufacturer. If you’ve been on a generic that works, don’t let the pharmacy change it to another brand. Ask them to fill it with the same one every time.
- Track your symptoms. Keep a simple log: date, dose, how you feel, any side effects. If you notice a change after a refill, show it to your doctor.
- Check inactive ingredients. If you have allergies (like to sulfites or lactose), use the FDA’s Inactive Ingredient Database to see what’s in each version. Many generics contain dyes or fillers that trigger reactions in sensitive people.
- Request therapeutic drug monitoring. For drugs like warfarin or phenytoin, ask for blood tests 3 to 5 days after any switch. Don’t wait for symptoms to appear.
Pharmacists at CVS and Walgreens now have protocols to block automatic substitution for NTI drugs unless the prescriber approves it. That’s progress. But it’s not universal. You still have to ask.
Is This a Problem for Everyone?
No. For most medications-like metformin for diabetes, or atorvastatin for cholesterol-the differences between generics and brands are meaningless. A 2020 review of 15 studies found no difference in HbA1c levels between generic and brand-name metformin. A 2024 study of 2.1 million patients found no increase in adverse events for 85% of drug classes.The issue isn’t generics. It’s the assumption that all drugs behave the same in all people. That’s not biology. That’s bureaucracy.
The Bigger Picture
The U.S. saves $373 billion a year on generics. That’s huge. But if we ignore individual variation, we trade short-term savings for long-term costs-more ER visits, hospitalizations, missed work, and failed treatments.Europe takes a different approach. The European Medicines Agency requires tighter bioequivalence ranges (90% to 111%) for NTI drugs. That means fewer generics get approved-but the ones that do are more predictable. In the U.S., we have more choices. But not always better outcomes.
Now, new tools are emerging. Pharmacogenomic testing can predict how your body metabolizes certain drugs with 83% accuracy. If you’re on multiple medications, this could help your doctor choose the right generic-or avoid one altogether.
For now, the system isn’t broken. It’s just blind. And if you’re one of the people who reacts differently, you have to be the one who speaks up.
Are generic medications always safe?
For most people, yes. Generic medications are safe and effective for the majority of drugs, especially those with wide therapeutic windows like metformin or statins. But for medications with narrow therapeutic indices-like levothyroxine, warfarin, or phenytoin-even small changes in absorption can cause serious side effects. The safety of a generic depends on the drug, not just the label.
Why do some people feel worse on generic levothyroxine?
Levothyroxine has a very narrow therapeutic range. Small differences in how the body absorbs the drug-due to different fillers, coatings, or dissolution rates-can cause thyroid hormone levels to shift. Studies show nearly a quarter of patients switching from brand-name Synthroid to generics experience abnormal TSH levels. Symptoms like fatigue, weight gain, or anxiety often follow. Many patients report feeling better after switching back to the same formulation they started on.
Can I be allergic to inactive ingredients in generics?
Yes. While the active ingredient is the same, generics can contain different dyes, preservatives, or fillers. For example, sodium metabisulfite, used as a preservative in some medications, triggers allergic reactions in 5-10% of asthmatic patients. Lactose, corn starch, or artificial colors can also cause issues in people with sensitivities. Always check the inactive ingredients list on the drug label or use the FDA’s Inactive Ingredient Database to compare formulations.
Should I ask my doctor to write "Do Not Substitute" on my prescription?
If you’re taking a narrow therapeutic index drug-like levothyroxine, warfarin, carbamazepine, or digoxin-yes. This prevents the pharmacy from automatically switching your generic without your doctor’s approval. Even if your insurance pushes for the cheapest option, your health comes first. Many pharmacists will honor this request, especially if you’ve had a bad reaction before.
What’s the difference between a generic and an authorized generic?
A regular generic is made by a different company and may have different inactive ingredients. An authorized generic is made by the original brand-name manufacturer but sold under a different label, often at a lower price. It’s chemically identical to the brand-name drug. For patients who’ve had problems with other generics, an authorized generic (like the FDA-approved version of Synthroid) can be a safer alternative without the high cost.
How can I tell if my generic medication is causing problems?
Keep a symptom journal. Note when you started a new batch of medication, what symptoms you’re experiencing, and whether they improved or worsened. For NTI drugs, blood tests (like TSH for thyroid meds or INR for warfarin) are the most reliable way to detect changes. If you feel different after a refill-even if it’s "the same drug"-don’t ignore it. Talk to your doctor and ask if a formulation change occurred.

13 Responses
Oh here we go again with the rich people crying because they can’t get their $200 brand-name thyroid pill while the rest of us survive on generics and still breathe. Wake up. You think your body is special? Everyone else takes generics and doesn’t turn into a zombie. This isn’t medicine, it’s privilege.
I had the exact same thing happen with my levothyroxine. I switched to a generic and suddenly couldn’t get out of bed. My brain felt like it was wrapped in cotton. I went to my doctor and he laughed. I told him I’d switch back to Synthroid and pay out of pocket if I had to. He didn’t laugh after I showed him my TSH levels. Now I get the same generic every time. Don’t let anyone tell you it’s all in your head. Your body knows.
generic is generic stop being weak
My grandma’s on warfarin and they switched her generic last month. She started bruising like a cartoon. Took her three days to get back to the old one. I looked up the inactive ingredients-turns out the new one had FD&C Red 40. She’s allergic to food dyes. No one thought to check. This isn’t conspiracy. It’s negligence. We need better tracking. Not just for thyroid meds, but for every drug people take daily.
Oh so now it’s the FDA’s fault? Funny how you blame the government but never mention that your doctor didn’t push back when the pharmacy switched you. Or that your insurance company forced the switch. Or that you didn’t check the label yourself. This isn’t about science. It’s about people refusing to take responsibility for their own health. If you don’t know what’s in your pill, you deserve what you get.
Europe does it better? Really? They have rationing. They wait months for prescriptions. We have choice. We have innovation. If you can’t handle a generic, go live in Sweden. America gives you the power to choose. Use it or shut up.
Wait, so you’re telling me that in Nigeria, we don’t even get generics? We get the real stuff? Or do we get nothing? I’ve seen people in Lagos swallow half a pill because they can’t afford the other half. You think your fatigue is bad? Try dying because your child’s asthma inhaler was too expensive. Your privilege is showing.
I used to be one of those people who thought generics were fine. Then I switched from brand-name bupropion to a generic and went full-on panic attack mode for two weeks. Couldn’t sleep. Started crying at commercials. My therapist said I was ‘overreacting.’ I switched back and felt like I’d been resurrected. Now I call the pharmacy every time. I ask for the exact manufacturer. I keep receipts. I’m not crazy. I’m just not a lab rat.
my doc said generic is same but i got a different one last month and now i feel like a zombie. i asked why and they said its because of the color. color??
Let’s be honest: this isn’t about bioequivalence. It’s about the pharmaceutical industry’s control over patient identity. The brand-name companies know that if you feel worse on a generic, you’ll blame yourself. They profit from your self-doubt. The FDA doesn’t care because they’re funded by the same companies. This is systemic gaslighting disguised as science.
It’s not just about the inactive ingredients-it’s about the lack of standardization across manufacturers. One company’s 80% bioavailability might be perfectly fine for a healthy 30-year-old, but for a 70-year-old with renal impairment? Catastrophic. The FDA’s one-size-fits-all model is a relic. We need individualized bioequivalence thresholds based on age, genetics, and comorbidities. Until then, we’re treating patients like data points, not humans.
Oh sweetie, you think you’re the first person to notice this? The FDA has known about this since the 90s. They just don’t want to admit it because it would cost billions to retest every generic. So they let you suffer quietly while they collect your tax dollars and your insurance premiums. And now you’re surprised? Honey, the system isn’t broken-it’s designed this way. You’re not special. You’re just the latest victim.
Thank you for this comprehensive and meticulously researched post. The distinction between active and inactive ingredients, particularly in narrow therapeutic index medications, is critically under-discussed in public health discourse. The data from JAMA Internal Medicine and the pharmacist survey are compelling and demand regulatory reform. Patients should be empowered with access to the FDA’s Inactive Ingredient Database, and prescribers must be educated on the clinical significance of formulation variability. A standardized, patient-centered approach to generic substitution is not merely advisable-it is an ethical imperative. This is not an issue of cost versus safety; it is a question of whether we value individual health outcomes as much as we value fiscal efficiency.