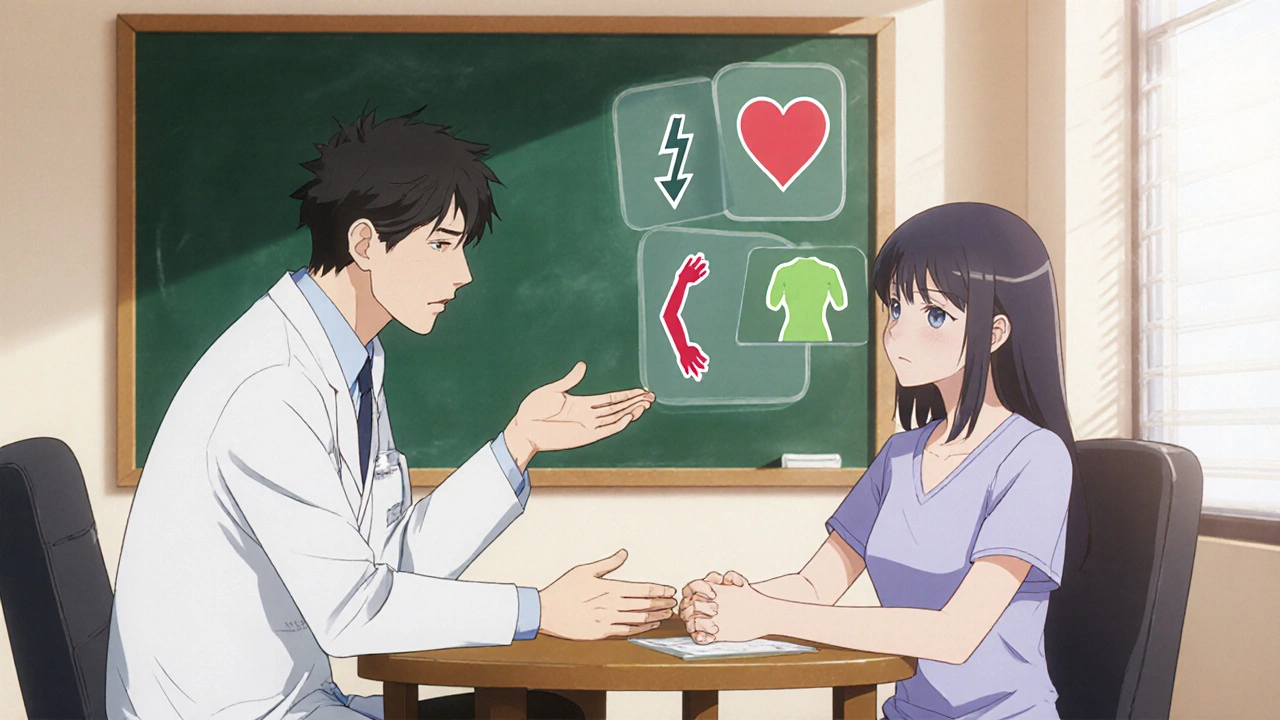
Side Effect Trade-Off Calculator
Compare Treatment Benefits and Side Effects
Enter the absolute risk numbers for both treatment benefits and side effects to calculate the trade-off ratio.
Calculation Method
Trade-off Calculation: The tool calculates the ratio of benefit to side effect risk. A ratio of 3:1 or higher typically indicates the benefit outweighs the risk for most patients.
For example, a 30% reduction in stroke risk with a 15% chance of nausea gives a ratio of 2:1 (30/15). With a 5% tolerance threshold, this would be considered acceptable.
Trade-Off Results
Based on your input, this treatment may be appropriate for you, but it's important to discuss your values and concerns with your healthcare provider.
When clinicians discuss medication options, Shared Decision-Making Scripts are structured conversation guides that help patients and providers weigh treatment benefits against potential side effects. These scripts turn a vague consent conversation into a clear, collaborative exchange, especially when the choice involves tricky side‑effect trade‑offs.
Imagine you’re starting a statin. The doctor says, “It lowers your heart risk,” but you’re terrified of muscle pain. Without a script, the talk ends quickly, and you may quit the medication later. With a well‑crafted script, the clinician asks what side effects matter most, explains exact probabilities, and together you decide if the benefit outweighs the risk. That’s the power of shared decision‑making (SDM) for side‑effect trade‑offs.
Why Side‑Effect Trade‑Offs Need a Script
Side‑effect concerns drive up to 86% of non‑adherence for statins and cause 3‑5% of anticoagulant users to stop therapy. Studies show that patients who receive structured SDM scripts experience a 23% drop in decisional conflict and a 29% reduction in treatment discontinuation (JAMA Internal Medicine, 2021). The script does three things:
- Clarifies risk numbers - absolute risks (e.g., 15% chance of nausea) instead of vague terms like “rare”.
- Frames the trade‑off - helps the patient weigh a 1‑in‑10 chance of severe bleeding against a 30% reduction in stroke risk.
- Documents the conversation - ensures the clinician records the patient’s risk tolerance in the electronic health record.
Core Frameworks Behind the Scripts
Two evidence‑based models dominate the field:
- SHARE Approach - developed by the Agency for Healthcare Research and Quality (AHRQ) in 2012. It breaks the conversation into five steps: Seek, Help, Assess, Reach, and Evaluate.
- Three‑Talk Model - championed by the American Academy of Family Physicians (AAFP) in 2022. It uses Option Talk, Discussion Talk, and Decision Talk, each with precise language for side‑effect data.
Both models stress clear numeric framing and patient values, but they differ in emphasis. SHARE is more step‑by‑step, while Three‑Talk focuses on conversational flow. Below is a quick side‑by‑side look.
| Aspect | SHARE Approach | Three‑Talk Model |
|---|---|---|
| Number of Steps | 5 (Seek, Help, Assess, Reach, Evaluate) | 3 (Option Talk, Discussion Talk, Decision Talk) |
| Typical Time Add‑on | ~7 minutes per visit (Scripps Health, 2022) | ~5-6 minutes (NICE oncology data, 2022) |
| Risk Framing Guidance | Absolute risk + visual aids (e.g., color‑coded charts) | Exact numeric statements (e.g., 1 in 10) |
| Patient‑Value Probe | “Which side effects would be deal‑breakers for you?” | “How much risk are you comfortable living with?” |
| Evidence of Effectiveness | 23% lower decisional conflict (MGH, 2023) | 78% clinicians report better adherence (NICE, 2022) |
Key Script Elements You Should Include
Regardless of the model you choose, a solid script contains four building blocks:
- Risk Presentation - Use absolute percentages and avoid terms like “rare”. Example: “15% of people on this drug report nausea.”
- Benefit Statement - Quantify the upside in the same units (e.g., “30% reduction in heart attacks”).
- Values Exploration - Ask open‑ended questions: “Which side effects would make you stop the medication?”
- Decision Summary - Restate the agreed plan and document the patient’s risk tolerance in the EHR.
Here’s a short, ready‑to‑use script excerpt for a new anticoagulant:
Clinician: “This medication lowers your stroke risk by about 30%, but it can cause bleeding in 3 out of 100 people. Some patients feel comfortable with that trade‑off, while others prefer a drug with a lower bleeding risk even if the stroke protection is a bit less. What concerns you most about bleeding or stroke?” Patient: “I’m worried about bleeding because I work a physically demanding job.” Clinician: “Understood. We can consider a lower‑dose option that reduces bleeding to 1 out of 100 but also lowers stroke protection to 20%. How does that sound?”
Implementing Scripts in Real‑World Practice
Getting scripts from paper to bedside is a multi‑step process:
- Training - A 4‑hour workshop (offered by the Massachusetts General Hospital Health Decision Sciences Center) with role‑playing reduces the learning curve. Clinicians reach proficiency after about 12 supervised encounters.
- Pre‑Visit Materials - Send patients a short video or pamphlet that explains side‑effect probabilities. This trims in‑visit time by ~3 minutes (Scripps Health data).
- EHR Integration - Use built‑in SDM modules (Epic Systems has them in 63% of U.S. hospitals) to auto‑populate the script and capture risk‑tolerance fields.
- Documentation - Record two key items: the side‑effect concerns voiced by the patient and the agreed risk threshold. The American Medical Association reports 68% adoption of these standards.
For busy primary‑care offices, start with a “light” version: use a one‑page checklist that captures the most critical trade‑offs and refer to the full script for complex cases like oncology or cardiology.
Common Pitfalls and How to Avoid Them
Even the best script can flop if misused. Here are three frequent mistakes and quick fixes:
- Reading the script verbatim - Patients notice when doctors sound robotic. Pause after each question, listen, and adapt the wording to the patient’s language.
- Over‑loading with numbers - Too many percentages confuse rather than clarify. Stick to two key risks and use visual aids for the rest.
- Skipping the values probe - Without asking what matters to the patient, you lose the shared‑decision spirit. Make the “deal‑breaker” question mandatory.
Addressing these issues can boost patient satisfaction by up to 41% (Scripps visual risk charts) and cut follow‑up calls about side‑effects by about one‑third.
Reimbursement and Policy Landscape
Since 2022, the AMA has introduced CPT codes 96170‑96171 for documented SDM encounters, reimbursing $45‑$65 per visit. Medicare Advantage plans must now record SDM for high‑risk medications (CMS, 2023). These policies make it financially viable to spend the extra 5-7 minutes on a thorough side‑effect discussion.

Future Directions: AI‑Assisted Scripts
Researchers at the National Institutes of Health are piloting natural‑language‑processing tools that listen to a patient’s words, flag hidden concerns (like “I’m scared of losing my independence”), and suggest real‑time script tweaks. Early trials show a 19% boost in uncovering unspoken worries, paving the way for smarter, more personalized SDM.
Quick Checklist for Running a Side‑Effect Trade‑Off Conversation
- Prepare absolute risk numbers for each side effect.
- Pick a framework (SHARE or Three‑Talk) and follow its sequence.
- Use visual aids (charts or infographics) for high‑impact risks.
- Ask the “deal‑breaker” question early.
- Summarize the decision and document risk tolerance in the EHR.
- Schedule a short follow‑up to reassess side‑effect experience.
Frequently Asked Questions
What exactly is a shared decision‑making script?
It is a pre‑written set of conversation prompts that guide clinicians and patients through a balanced discussion of benefits, risks, and personal values, especially when side effects are a major concern.
How long does a typical side‑effect trade‑off conversation take?
Studies show an average add‑on of 5-7 minutes per visit when using a structured script, though pre‑visit educational videos can shave a few minutes off the in‑office time.
Which framework should I pick: SHARE or Three‑Talk?
If your setting values a step‑by‑step checklist, go with SHARE. If you prefer a smoother conversational flow, the Three‑Talk model may feel more natural. Both achieve similar outcomes when applied correctly.
Do insurance plans pay for these longer conversations?
Yes. CPT codes 96170‑96171 reimburse clinicians for documented SDM encounters, and many Medicare Advantage plans now require SDM documentation for high‑risk meds.
Can I use these scripts for emergency situations?
Full scripts are hard to fit into emergent care; only a rapid “key‑risk” version is feasible. Research shows only 12% of emergency visits can accommodate complete SDM.
Implementing well‑crafted shared decision‑making scripts transforms vague consent into a partnership that respects patient values while keeping clinicians on track. By following the steps above, you’ll cut decisional conflict, improve adherence, and meet emerging reimbursement standards. shared decision-making scripts aren’t just paperwork - they’re a proven tool for safer, patient‑centered care.

11 Responses
When I first walked into the clinic, I felt like I was stepping onto a stage where fate itself was holding the script in trembling hands.
The doctor tried to explain the statin, but the words sounded like distant thunder echoing through a canyon of doubt.
Every side‑effect floated like a specter, each one tugging at my nerves with the intensity of a drama queen demanding the spotlight.
I could almost hear the chorus of my own fears chanting “muscle pain” louder than any promise of reduced heart risk.
Then the shared decision‑making script burst onto the scene like a heroic narrator, offering clarity where chaos reigned.
The script laid out the numbers in bright, unambiguous figures, turning vague threats into concrete probabilities that I could actually grasp.
It asked me which outcomes I could tolerate, inviting me to become the protagonist of my own health story rather than a passive extra.
With each question, the tension loosened, and I felt the weight of uncertainty lift like a curtain being drawn back.
The clinician didn’t just read a list; they paused, listened, and adjusted the language to match my own rhythm, a true duet of minds.
By the end of the conversation, the trade‑off no longer felt like a cruel bargain but a balanced partnership, each side aware of the stakes.
I left the office with a plan that felt both courageous and realistic, a script‑guided oath to follow up on side‑effects and adjust as needed.
The whole experience reminded me that medicine is not merely a set of pills but a narrative we co‑author, chapter by chapter.
In the weeks that followed, I noticed the muscle aches eased, not because the drug was magical, but because I had mentally prepared for them and knew when to speak up.
When the nurse documented my risk tolerance, it felt like a signed contract between my values and my physician’s expertise.
And that, dear readers, is why the drama of side‑effect trade‑offs demands a script – without it, the story collapses into chaos.
Hey team this is a solid blueprint for risk stratification and patient engagement.
Using shared decision‑making scripts leverages evidence based communication and boosts adherence metrics.
The framework turns abstract pharmacodynamics into patient friendly numbers.
It empowers patients to align therapeutic goals with personal values.
Roll this out and watch satisfaction scores climb.
Listen up the script isn’t a suggestion it’s a must if you want patients sticking to meds.
Don’t waste time vague talk just throw the numbers out straight.
Ask the deal‑breaker question early and you’ll cut the back‑and‑forth in half.
Stick to the plan and watch the quit rates drop.
Enough talk get it done.
I appreciate the thorough breakdown of the SHARE steps.
It’s clear how each phase builds on the previous one, making the conversation flow naturally.
One practical tip is to use a visual aid during the risk presentation to keep patients focused.
Also, scheduling a brief follow‑up call can catch side‑effects early and reinforce the decision.
Overall this approach nicely balances structure with flexibility.
Oh great, another script to add to the already overflowing paperwork mountain.
Honestly this whole push for scripted consent feels like a desperate attempt to cover up the medical industry’s habit of downplaying risks.
We should be demanding full transparency outright, not hiding behind polished talking points.
Patients deserve the raw truth and we shouldn’t sugarcoat the potential harms just to hit a compliance checkbox.
It’s time to call out the paternalistic tone and demand real empowerment.
Isn’t it fascinating how a simple checklist can become a mirror reflecting our deepest anxieties about control and agency? 😊
When we articulate risks in numbers, we’re essentially translating uncertainty into a language we can manipulate.
But does that demystify the fear or merely relocate it onto the page? 🤔
Perhaps the true power lies not in the script itself but in the shared silence that follows, where both doctor and patient breathe in the same uneasy truth.
In any case, a well‑crafted script is a tool, not a talisman. 😄
From a systems perspective the integration of SDM modules into EHRs reduces duplication and aligns with interoperability standards.
Even with low punctuation the core message stays intact – data capture meets compliance and improves patient‑centred outcomes.
Overall seems like a win‑win.
I’ve seen clinics that adopted these scripts see a noticeable dip in medication discontinuation rates, often around 20‑30 %.
One practical approach is to embed the risk‑tolerance fields directly into the after‑visit summary so the patient can review them at home.
If you’re concerned about time constraints, consider handing out a pre‑visit video that walks through the key numbers – it shaves off a few minutes during the actual encounter.
Feel free to reach out if you need template resources or advice on customizing the visual aids for your patient population.
What if the push for SDM scripts is just another layer of control built into the system to keep us docile
we are being fed polished talking points while the real agenda stays hidden behind CPT codes
the truth is masked by the jargon and the numbers become a veil for manipulation
question everything and look beyond the approved scripts
Dear colleagues your dedication to embedding shared decision‑making into practice is commendable 😊
Remember that the essence of coaching lies in guiding patients to discover their own values rather than imposing a preset choice.
By framing risk with both absolute and relative metrics you empower them to make informed decisions.
Let us continue to refine our scripts, ensuring they remain flexible yet evidence‑based 😇
Together we can elevate patient autonomy while maintaining clinical rigor.