Beta-Blocker Psoriasis Risk Calculator
Psoriasis Risk Assessment
Your Psoriasis Risk Assessment
Recommendations:
For millions of people managing high blood pressure or heart conditions, beta-blockers are a lifeline. But if you also have psoriasis, these common drugs might be quietly making your skin worse - sometimes dramatically so. It’s not a rumor. It’s not just anecdotal. Doctors and researchers have been seeing this pattern for decades, and the evidence keeps growing.
What’s Actually Happening Between Beta-Blockers and Psoriasis?
Beta-blockers like metoprolol, propranolol, and atenolol work by slowing your heart rate and lowering blood pressure. They do this by blocking adrenaline from binding to beta receptors in your heart and blood vessels. But those same receptors are also found in your skin. When beta-blockers interfere with them there, they disrupt how skin cells grow and how your immune system reacts.
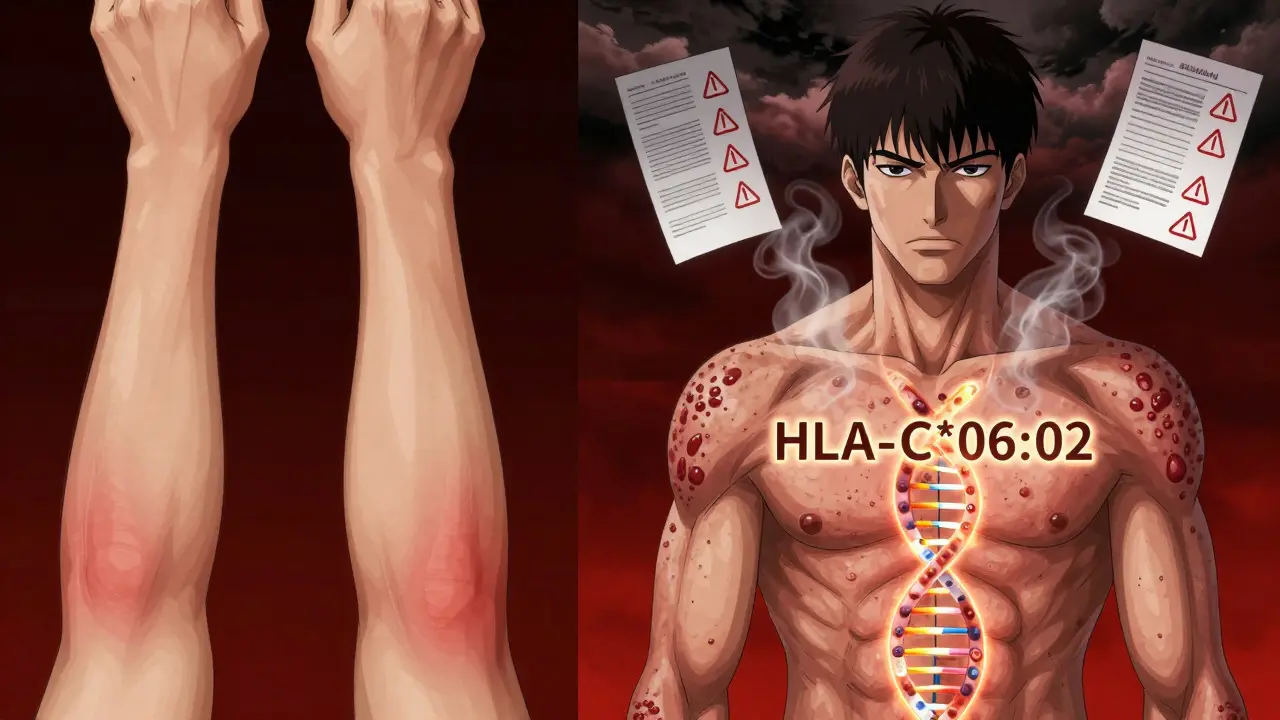
The result? A flare-up. For people who already have psoriasis, this often means thicker plaques, more itching, or even a sudden shift from regular plaque psoriasis to pustular psoriasis - a more severe form with pus-filled bumps. In some cases, people who never had psoriasis before develop it after starting a beta-blocker. The timing is tricky: it can show up as early as one month after starting the drug, or as late as 18 months later. That delay is why many patients never connect their skin flare to their heart medication.
Research from DermNet NZ and Banner Health shows about 20% of people with existing psoriasis see their condition worsen on beta-blockers. And it’s not just oral pills. Even eye drops like timolol - used for glaucoma - can cause flare-ups because enough of the drug gets absorbed into the bloodstream to affect the skin.
Which Beta-Blockers Are the Worst Offenders?
Not all beta-blockers are created equal when it comes to skin risk. Some carry a much higher chance of triggering psoriasis than others.
- Propranolol - often linked to severe flares and new-onset psoriasis
- Metoprolol - the most commonly prescribed beta-blocker in the U.S., and one of the top triggers reported by dermatologists
- Atenolol - associated with pustular psoriasis in case studies
- Pindolol - known to transform plaque psoriasis into pustular forms
- Timolol - topical version, but still causes systemic skin reactions
Interestingly, older beta-blockers like practolol were pulled from the market in the 1980s because so many patients developed psoriasiform rashes. That’s not a coincidence - it’s a warning sign that was ignored for too long.
Why Do Some People Get Flares and Others Don’t?
This is where things get complicated. Two people on the same dose of metoprolol can have completely different outcomes. One stays clear. The other’s skin explodes.
Genetics may be the key. A 2024 study at Johns Hopkins and Mayo Clinic found that people with the HLA-C*06:02 gene variant - already known to increase risk for psoriasis - are far more likely to have a flare triggered by beta-blockers. This isn’t a guarantee, but it’s a strong clue. If you have a family history of psoriasis or tested positive for this gene, you’re at higher risk.
Other factors matter too. Stress, infections, alcohol, and even cold weather can combine with beta-blockers to push your skin over the edge. And while some studies suggest cumulative exposure doesn’t matter much, real-world patient reports tell a different story: the longer you’re on the drug, the more likely a flare becomes.
What Does the Science Say? Contradictions and Consensus
There’s conflicting data. A 2010 study in the Journal of the American Academy of Dermatology found beta-blockers to be a “major factor” in triggering or worsening psoriasis in hospitalized patients. But another paper from the same year concluded that overall drug exposure wasn’t a strong risk factor. So which is right?
The answer is both - depending on who you’re looking at. For the general population, the risk might be low. But for someone with psoriasis, especially if they carry certain genes, the risk is real and significant. The American Academy of Dermatology’s 2022 position statement puts it plainly: beta-blockers are among the most common drug classes linked to psoriasis flares.
And here’s the clincher: when patients stop taking the drug, their skin often improves. That’s the clearest sign the medication was the trigger. If your psoriasis clears up after switching medications, that’s not luck - it’s evidence.
What Should You Do If You’re on Beta-Blockers and Have Psoriasis?
If you’re on a beta-blocker and notice your skin getting worse, don’t panic. But don’t ignore it either. Talk to both your cardiologist and dermatologist. This isn’t a decision you should make alone.
Here’s what to ask:
- Could my current beta-blocker be making my psoriasis worse?
- Is there a safer alternative for my heart condition?
- Would switching to a calcium channel blocker (like amlodipine) or an ARB (like losartan) be a good option?
Yes, some other blood pressure meds can also trigger psoriasis - ACE inhibitors, for example. But beta-blockers are the most consistently linked. And if one beta-blocker caused a flare, chances are another will too. Most doctors won’t try a different one.
Meanwhile, manage your skin with proven treatments: topical steroids, vitamin D creams, or light therapy. For severe cases, biologics or oral medications might be needed. But fixing your skin won’t work if you’re still on the drug triggering it.

Real Stories: What Patients Are Saying
Online communities like MyPsoriasisTeam and Reddit’s r/psoriasis are full of stories that mirror the clinical data.
One user wrote: “I started metoprolol for anxiety-related palpitations. Six months later, my scalp and elbows were covered. I didn’t make the connection until my dermatologist asked if I was on beta-blockers.”
Another said: “I’ve had mild psoriasis for years. After switching to propranolol for high blood pressure, my body looked like a map of red patches. I went from 5% coverage to 30% in three months.”
But not everyone has problems. Some users report no change at all. That’s why blanket warnings don’t work. But for the 1 in 5 who are affected, the impact is life-altering.
What’s Next? Research and Hope
Scientists are working on better solutions. New beta-blockers are being designed to target only the heart’s beta-1 receptors, avoiding skin receptors entirely. If successful, these could be game-changers for people with psoriasis who need heart medication.
Genetic testing may soon become part of routine care. If you’re prescribed a beta-blocker and have psoriasis, a simple DNA test could tell you whether you’re at higher risk - and help your doctor choose a safer alternative before the flare even starts.
In the meantime, awareness is the best tool you have. If you have psoriasis and are on any kind of beta-blocker, pay attention to your skin. Track changes. Keep a photo journal. Bring it up at your next appointment. You’re not overreacting. You’re being smart.
Frequently Asked Questions
Can beta-blockers cause psoriasis in someone who never had it before?
Yes. While beta-blockers are more likely to worsen existing psoriasis, they can also trigger new-onset psoriasis in people who never had it. Studies and case reports show this happens, especially with drugs like propranolol and metoprolol. The process can take months, so it’s easy to miss the connection.
If one beta-blocker causes a flare, will others do the same?
Very likely. Most dermatologists and cardiologists agree that if you had a flare with one beta-blocker, switching to another one in the same class probably won’t help. The mechanism is similar across these drugs. The safer move is to switch to a different class of blood pressure medication altogether.
Are there blood pressure meds that are safer for psoriasis patients?
Yes. Calcium channel blockers like amlodipine and angiotensin receptor blockers (ARBs) like losartan are generally considered safer alternatives. ACE inhibitors can still trigger psoriasis in some people, so they’re not always the best choice. Your doctor can help weigh your heart health needs against your skin condition.
How long does it take for psoriasis to improve after stopping a beta-blocker?
It varies. Some people see improvement within weeks. Others take a few months. The skin needs time to reset after the drug is cleared from the system. If your flare doesn’t improve after 2-3 months off the medication, other triggers may be involved - and your dermatologist can help identify them.
Can eye drops for glaucoma cause psoriasis flares?
Yes. Timolol eye drops, commonly used for glaucoma, can be absorbed through the eye and enter the bloodstream. There are documented cases where patients developed or worsened psoriasis after using these drops. If you’re using timolol eye drops and have psoriasis, tell your dermatologist. There are alternative glaucoma medications with lower risk.


8 Responses
Been on metoprolol for 5 years with mild psoriasis. Didn’t think much of it until my elbows started flaring like crazy last winter. Switched to amlodipine after my derm asked if I was on beta-blockers - and yeah, my skin’s been calm for 8 months now. Not saying it’ll work for everyone, but if you’re struggling and your meds haven’t changed, it’s worth a chat with your doc. You’re not crazy for noticing a pattern.
Also, psoriasis isn’t just ‘dry skin.’ It’s immune chaos. And sometimes, the thing keeping your heart alive is making your skin scream.
The HLA-C*06:02 association is the most clinically significant finding here. This isn’t just pharmacokinetics - it’s pharmacogenomics in action. Beta-blockers modulate cAMP pathways in keratinocytes, and in genetically predisposed individuals, this disrupts IL-23/Th17 axis regulation. The fact that topical timolol can trigger systemic flares underscores the bioavailability issue - ocular absorption bypasses first-pass metabolism, delivering active drug directly to dermal beta-receptors.
Most cardiologists still treat this as anecdotal, but the 2024 Mayo study with SNP arrays should change that. We need pre-prescription genotyping for high-risk dermatology patients. It’s not overkill - it’s precision medicine.
It is of paramount importance to acknowledge that the pharmaceutical industry has, for decades, prioritized efficacy metrics over dermatological safety profiles in the development of cardiovascular therapeutics. The continued prescription of beta-blockers in populations with known psoriatic diathesis represents not merely a clinical oversight, but an ethical lacuna in patient-centered care. The burden of proof should not rest upon the patient to connect the dots between a medication and a chronic inflammatory condition - rather, it ought to be incumbent upon prescribers to conduct comprehensive risk-benefit analyses prior to initiation.
Furthermore, the omission of psoriasis as a contraindication in FDA labeling is a glaring regulatory failure.
Okay but what if beta-blockers are actually helping your psoriasis and the doctors are lying? I read on a forum that the FDA is in cahoots with Big Pharma to keep people on steroids and biologics because they make more money that way. My cousin’s neighbor’s dog got psoriasis after a beta-blocker, but then it went away when he started taking vitamin D3 and wearing copper bracelets. Coincidence? I think not.
Also, did you know timolol eye drops are used by the government to track people’s immune responses? It’s in the patent filings. Look it up.
I’ve had plaque psoriasis since I was 19. Started metoprolol for PVCs at 32. Didn’t notice anything until my scalp started flaking like crazy six months in. My derm asked if I was on beta-blockers - I didn’t even think to mention it. We switched to losartan and within 10 weeks, my skin was 80% better. I wish I’d known sooner. This post saved me months of frustration.
For anyone reading this: keep a photo journal. Even one picture a month helps your doctor see the trend. And don’t be afraid to ask for alternatives. Your skin matters too.
I just want to say - if you’re reading this and you’re scared because your skin’s acting up and you’re on beta-blockers, you’re not alone. I was terrified when my hands started pustulating. I thought I was losing my mind. I didn’t tell my cardiologist for months because I didn’t want to seem like a hypochondriac. But when I finally did, he didn’t brush me off. He said, ‘Let’s try something else.’
It took three months for my skin to calm down after switching to amlodipine. I cried when I saw my palms for the first time without those angry red bumps. This isn’t just about medication - it’s about being heard. So if you’re feeling dismissed? Keep pushing. You’re not overreacting. Your body’s screaming. Listen to it.
I started propranolol for migraines and my psoriasis went full nuclear. Took me 8 months to connect the dots. Switched to verapamil. Skin’s chill now. Just saying.
In India, we rarely see this discussed in clinics. Beta-blockers are cheap, accessible, and prescribed without skin history checks. I’ve seen patients with severe pustular psoriasis on metoprolol, and doctors blame it on ‘stress’ or ‘diet.’ But this isn’t about lifestyle - it’s pharmacology. We need awareness campaigns in vernacular languages. A patient in rural Punjab shouldn’t have to Google this in English to save their skin.
Also, timolol eye drops are sold over the counter here. No prescription. No warning. This is a public health blind spot.