Immunosuppressant Probiotic Risk Assessment Tool
This tool helps you assess your risk of probiotic-related infections based on your immunosuppression status and other factors. Results are based on guidelines from the Infectious Diseases Society of America.
Risk Assessment Guide
Neutropenia (<500), recent stem cell transplant, central lines
Solid organ transplant <3 months, multiple immunosuppressants
Stable autoimmune disease on one drug, CD4 >200
No immunosuppression or mild treatment
Your personalized risk assessment will appear here after calculation.
When you're on immunosuppressants-whether after a transplant, for autoimmune disease, or during chemotherapy-your body is already playing defense. Your immune system is turned down on purpose. That’s why you’re less likely to reject a new organ or flare up with rheumatoid arthritis. But this same protection can make you vulnerable in ways you might not expect. One of those unexpected risks? Probiotics.
Probiotics are often seen as harmless, even helpful. They’re in yogurt, capsules, powders. Ads tell you they boost digestion, strengthen immunity, balance gut flora. But for someone on immunosuppressants, those "good" bacteria and yeasts can turn dangerous. In rare but serious cases, they can escape the gut, enter the bloodstream, and cause life-threatening infections like sepsis, fungemia, or endocarditis. This isn’t theoretical. Between 2000 and 2020, 47 documented cases of probiotic-related infections occurred, and 83% of them happened in people with weakened immune systems. Nearly one in three of those cases ended in death.
Why Probiotics Can Be Risky When Your Immune System Is Suppressed
Probiotics aren’t medicines. They’re live microorganisms-mostly bacteria like Lactobacillus and Bifidobacterium, or yeast like Saccharomyces boulardii. In healthy people, these microbes stay mostly in the gut. They help crowd out bad bacteria, support the gut lining, and even talk to immune cells. But in someone on immunosuppressants, that barrier can break. The gut lining gets leaky. The immune system can’t respond fast enough. And suddenly, a microbe meant to help becomes a pathogen.
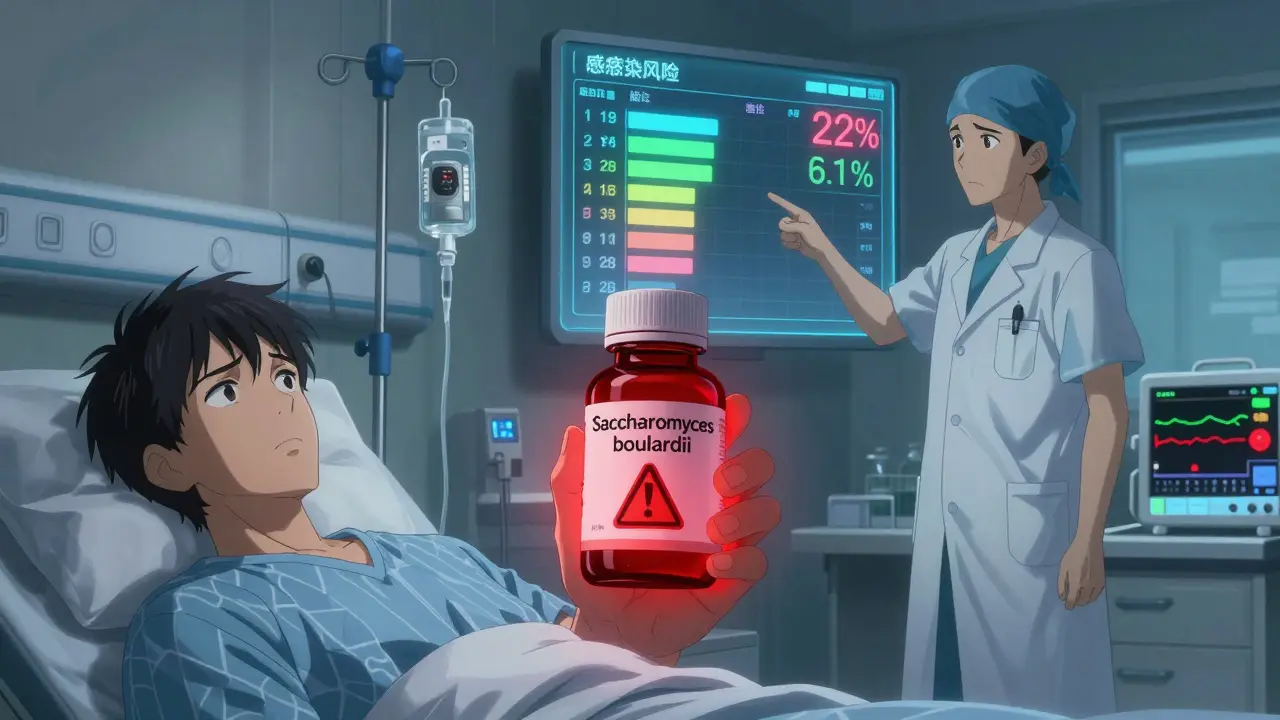
It’s not just any probiotic. The risk varies wildly by strain. Saccharomyces boulardii, a yeast often used for diarrhea, is especially dangerous. It’s been linked to 12 of the 47 known infection cases. When combined with a central venous catheter-a tube in a big vein used for IV meds or nutrition-the risk of bloodstream infection jumps. One 2019 study found a 27% higher chance of catheter-related infection in patients taking S. boulardii. And the fatality rate? Up to 22% in documented cases.
Even common strains like Lactobacillus rhamnosus GG (used in many supplements) have caused bacteremia in transplant patients. In one case series, three patients on immunosuppressants for autoimmune diseases developed Lactobacillus sepsis after taking probiotics. Two ended up in the ICU.
Who’s at the Highest Risk?
Not everyone on immunosuppressants is equally at risk. Your danger level depends on how weak your immune system is and what kind of treatment you’re getting.
- Neutropenia (ANC <500 cells/µL): If your white blood cell count is this low-common during chemotherapy-your body can’t fight off even small invasions. Probiotics are strictly avoided in this group at 87% of U.S. cancer centers.
- Recent transplant (first 3 months): Right after a liver, kidney, or heart transplant, immunosuppression is at its peak. In bone marrow transplant patients, probiotic use has been tied to a 4.2-fold increase in bloodstream infections.
- Central venous catheters: Any tube going into a major vein is a direct path for microbes. Combine that with S. boulardii, and you’ve got a perfect storm.
- Severe HIV (CD4 <100): People with advanced HIV have a 3.8 times higher risk of fungal infections from probiotics. But those with CD4 counts above 200 show minimal risk.
On the other end, some patients do fine. A 2022 meta-analysis of liver transplant patients found probiotics actually reduced bacterial infections by 34%-with no increase in serious side effects. That’s because liver transplant patients often have gut issues from antibiotics and bile changes, and certain strains may help restore balance without crossing the barrier.
What the Experts Say-And Why It’s Confusing
There’s no single answer. Guidelines clash. Some say avoid probiotics entirely. Others say use them cautiously under supervision.
The European Society for Clinical Nutrition and Metabolism (ESPEN) says: Don’t use probiotics in critically ill or immunocompromised patients. Strong recommendation. Moderate evidence.
The American Gastroenterological Association (AGA) says: It’s okay to use specific strains like Lactobacillus or Bifidobacterium for hepatic encephalopathy in cirrhosis patients. Weak recommendation. Low evidence.
Dr. V. Stadlbauer, a researcher in Austria, points out that in HIV patients and post-surgery cases, probiotics appear safe. But for bone marrow and solid organ transplants, safety is still a concern.
Meanwhile, companies like Optibac Probiotics say: We don’t recommend live cultures for immunosuppressed people. No clinical proof of benefit. Too much risk.
The disconnect? Probiotics aren’t regulated like drugs. The FDA treats them as dietary supplements. That means no pre-market safety review for high-risk groups. A bottle of probiotics can say "10 billion CFUs" without proving what’s actually inside, or whether those strains are safe for someone on tacrolimus.
When Probiotics Might Be Safe-And How to Use Them Wisely
If you’re on immunosuppressants and want to try probiotics, don’t quit cold turkey. Don’t start blindly. Do this instead:
- Know your risk category: Use the Infectious Diseases Society of America’s four-tier system:
| Category | Risk Level | Recommendation |
|---|---|---|
| 1 | Extreme | Absolute contraindication: Neutropenia <500, recent stem cell transplant, central lines |
| 2 | High | Use only with infectious disease consultation: Solid organ transplant <3 months, multiple immunosuppressants |
| 3 | Moderate | Selective use: Stable autoimmune disease on one drug, CD4 >200 |
| 4 | Low | Standard use: No immunosuppression |
- Choose single-strain products: Multi-strain probiotics have 63% higher risk of translocation. Stick to one strain with documented safety-like Lactobacillus rhamnosus GG ATCC 53103 or Bifidobacterium longum 35624.
- Avoid Saccharomyces boulardii: This yeast is the most dangerous. Even if your doctor says it’s okay, ask: "Is there a bacterial alternative?"
- Track your symptoms: If you develop a fever over 101°F, stop immediately. Get blood cultures. Don’t wait.
- Ask for strain-specific documentation: Don’t just say "a probiotic." Ask for the exact strain name and lot number. Different strains of the same species behave differently.
What About Alternatives?
If probiotics feel too risky, you’re not out of options. A new class called postbiotics is emerging. These are not live microbes. They’re inactivated bacterial cells or the beneficial compounds they produce-like short-chain fatty acids or enzymes. A 2023 clinical trial (NCT04873011) showed postbiotics reduced C. difficile infections in immunocompromised patients by 40%, with zero infections caused by the treatment itself.
Another option? Prebiotics. These are fibers that feed your own good bacteria. Foods like garlic, onions, asparagus, and oats can help without introducing foreign microbes. They’re safe, natural, and don’t carry infection risk.
For gut symptoms, some doctors now recommend low-FODMAP diets or targeted antibiotics for SIBO instead of probiotics. It’s not glamorous, but it’s proven.

What’s Changing in 2025?
Things are shifting fast. In July 2023, the FDA required warning labels on all probiotics containing Saccharomyces boulardii for immunocompromised patients. That’s a big deal-it’s the first time they’ve acted on this issue.
The PROTECT registry, launched in 2023, is tracking 5,000 immunosuppressed patients across 47 hospitals. Preliminary results are expected in mid-2025. This could finally give us clear, evidence-based rules-not guesswork.
Also, pediatric guidelines changed in January 2024. ESPGHAN now warns that 78% of probiotic infections in children happen in those with inflammatory bowel disease on biologic drugs. That means parents and pediatricians need to be just as cautious as adults.
Bottom Line: Don’t Guess. Ask.
Probiotics aren’t evil. For most people, they’re safe and helpful. But if you’re on immunosuppressants, they’re not a wellness trend. They’re a medical decision.
Don’t rely on Instagram advice. Don’t follow what a Reddit user said. Talk to your doctor. Ask: "Is this safe for my specific immune status?" Show them the label. Ask which strain you’re taking. Ask if there’s a postbiotic alternative.
One patient, on methotrexate for rheumatoid arthritis, took a single-strain probiotic for three years with no issues. Another, after a kidney transplant, got sepsis from the same kind of supplement. The difference? One had medical oversight. The other didn’t.
Your immune system is already doing a lot. Don’t make it fight an invisible battle it wasn’t designed to win.
Can I take probiotics if I’m on prednisone?
It depends. Prednisone alone is lower risk than combinations like prednisone + mycophenolate. If you’re on a single low dose and have no other risk factors (like a catheter or recent transplant), your doctor might allow a single-strain probiotic like Lactobacillus rhamnosus GG. But avoid Saccharomyces boulardii completely. Always get clearance from your care team.
Are probiotics safe after a kidney transplant?
In the first three months after a kidney transplant, probiotics are generally not recommended. Your immune suppression is strongest then. After that, some centers allow specific strains under close monitoring, especially if you have chronic diarrhea or gut issues. Never start without consulting your transplant team and an infectious disease specialist.
Do probiotics interfere with immunosuppressant drugs?
Probiotics don’t directly interact with drugs like cyclosporine or tacrolimus. But they can change your gut environment, which might affect how your body absorbs those medications. More importantly, if a probiotic causes an infection, your body will need stronger treatment-possibly more immunosuppressants or antibiotics-which can complicate your overall care.
What should I look for on a probiotic label if I’m immunosuppressed?
Avoid products with Saccharomyces boulardii. Look for single-strain formulas with exact strain names (e.g., Lactobacillus rhamnosus GG ATCC 53103). Avoid multi-strain blends. Check for third-party testing (USP or NSF certified). If the label just says "probiotic blend" without strain details, don’t take it.
Is there a probiotic that’s proven safe for transplant patients?
No probiotic is universally "safe" for all transplant patients. But in liver transplant recipients, certain strains like Lactobacillus plantarum and Bifidobacterium infantis have shown benefit without increased infection risk in clinical trials. Even then, they’re used under strict supervision. Always assume any live microbe carries risk unless your medical team says otherwise.
Can I get probiotics from food instead of supplements?
Fermented foods like yogurt, kefir, sauerkraut, and kimchi contain live cultures-but they’re not standardized. The strains and amounts vary widely. For high-risk patients, even food-based probiotics are often avoided. If you want to eat fermented foods, talk to your doctor first. Pasteurized versions (like cooked sauerkraut) are safer because they contain no live microbes.


13 Responses
I read this and thought: wow, probiotics are basically tiny traitors in your gut. Like, you think you're doing something healthy, but nope-those little bacteria are just waiting to turn on you. I mean, I used to eat that yogurt every day. Now I'm just... scared.
This article is a masterclass in medical nuance-and yet, the public still treats probiotics like vitamins. People don’t understand that 'natural' doesn’t mean 'safe.' The FDA treats them like candy, not pathogens. And we wonder why hospitals are full of iatrogenic infections? It’s not negligence-it’s negligence dressed up as wellness.
I bet this is all Big Pharma’s fault. They don’t want you to heal naturally, so they scare you off probiotics so you’ll keep buying their $500-a-month drugs. My cousin took probiotics after chemo and lived to 87. They’re just trying to control the narrative.
So... we’re supposed to trust doctors who can’t even agree if probiotics are bad or good? 😅 Meanwhile, my gut’s doing the tango with a yeast that might be trying to colonize my bloodstream. Thanks, science.
In india we have curd and buttermilk for generations and no one dies from it. Why now suddenly probiotics are dangerous? Maybe its the supplement industry making up fear to sell something else
Hey everyone-just wanted to say this is one of the most thoughtful pieces I’ve read on this topic. 🙏 If you’re immunocompromised, please don’t panic-but please also don’t treat your gut like a science experiment. Talk to your care team. Your health is worth the call.
Probiotics are just bacteria. Bacteria live everywhere. Your skin has more than your gut. So why are we acting like this is a new threat? The real issue is overmedication and fearmongering
The fact that you can buy a jar of 'immune boosting' yeast at CVS and it’s not regulated like a drug is a joke. This isn’t health-it’s capitalism with a smiley face.
I’ve been on tacrolimus for 8 years. Took L. rhamnosus GG for a year with no issues. My doctor approved it. Everyone’s risk is different. Don’t let fear override your own experience.
Let’s be real-most people who take probiotics don’t even know what strain they’re taking. The labels are designed to confuse. If you can’t pronounce it, don’t swallow it. Simple.
My mom took probiotics after her transplant and got sepsis. They said it was 'rare' but it happened to her. Now she’s scared to eat yogurt. I get it. But what about all the people who are fine? Why don’t they get heard?
I think the real question isn’t whether probiotics are dangerous-but whether we’re asking the right questions. Are we treating the gut as a separate system? Or are we finally starting to see it as part of the immune landscape? Maybe the answer isn’t avoidance-it’s understanding.
I’m from Nigeria, and we’ve always used fermented foods-no supplements, no hype. Just food. Maybe the answer isn’t more science, but returning to what our grandmothers knew: real food, simple, safe. 🌱💛