Pregnancy Vaccination Timing Guide
Personalized Prophylaxis Plan
Enter your current pregnancy stage to receive vaccination timing recommendations based on evidence-based guidelines.
Recommended Vaccinations:
Why This Timing Matters
Key Benefits
Expecting a baby brings a flood of decisions, and one that often slips under the radar is how to protect both mom and baby from preventable illnesses. pregnancy prophylaxis isn’t just a buzzword-it’s a set of evidence‑based actions that keep infections at bay, reduce complications, and support a smoother pregnancy journey.
What Does Prophylaxis Mean in Pregnancy?
Prophylaxis in Pregnancy is a preventive strategy that uses vaccines, medications, or lifestyle measures to avoid infections and medical complications during gestation. The goal is simple: stop problems before they start. This differs from treatment, which kicks in after an issue is identified.
Why Prophylaxis Matters for Expecting Mothers
Pregnancy changes a woman’s immune system, making her more susceptible to certain germs. At the same time, the developing fetus is vulnerable to infections that can cross the placenta. Effective prophylaxis lowers the risk of miscarriage, preterm birth, congenital anomalies, and severe maternal illness.
Core Prophylactic Measures Every Pregnant Woman Should Know
- Vaccinations (influenza, Tdap, hepatitis B, and more)
- Antibiotic prophylaxis for specific infections (e.g., Group B Streptococcus)
- Antimalarial prophylaxis when traveling to endemic regions
- Thromboprophylaxis to prevent blood clots
- Nutrition‑based prevention (prenatal vitamins, safe food handling)
Each of these measures targets a different threat, but together they form a comprehensive safety net.
Vaccination: The First Line of Defense
Influenza vaccine is a seasonal inactivated vaccine recommended for all pregnant women, ideally before the start of the flu season. Flu can cause severe pneumonia in pregnant women and is linked to premature labor. Studies from the CDC (2023) show a 50% reduction in flu‑related hospitalization when the vaccine is administered during pregnancy.
Tdap vaccine (tetanus, diphtheria, pertussis) is given between 27 and 36 weeks of gestation to protect newborns from whooping cough. Pertussis can be fatal for infants under two months, and maternal antibodies passed through the placenta provide critical early protection.
Other vaccines often discussed include hepatitis B (for high‑risk mothers), COVID‑19 (aligned with latest WHO guidance), and the newly approved RSV vaccine for pregnant women (2024). All are safe during any trimester, though timing may vary.
Antibiotic Prophylaxis: Targeted Infection Prevention
Group B Streptococcus (GBS) screening involves a rectovaginal swab at 35‑37 weeks; if positive, intrapartum intravenous antibiotics (usually penicillin) are given to prevent neonatal sepsis. The protocol reduces early‑onset GBS disease by >80%.
For women with a history of urinary tract infections, a short course of nitrofurantoin or fosfomycin in the second trimester can lower recurrence rates, but only under physician supervision.
Travel‑Related Prophylaxis: Malaria and Beyond
Malaria prophylaxis is essential for pregnant travelers to endemic areas, typically using artemisinin‑based combination therapy (ACT) after the first trimester, followed by weekly chloroquine or mefloquine when appropriate. Malaria in pregnancy raises the risk of severe anemia, low birth weight, and fetal loss. The WHO recommends avoiding travel to high‑risk zones during the first trimester whenever possible.
Other travel‑related measures include typhoid vaccination, avoiding raw foods, and thorough hand hygiene.
Thromboprophylaxis: Guarding Against Blood Clots
Thromboprophylaxis involves low‑dose aspirin (81 mg daily) for women with a history of preeclampsia, thrombophilia, or multiple pregnancy, and low‑molecular‑weight heparin for those with confirmed clotting disorders. Studies from the Royal College of Obstetricians (2022) indicate a 30% drop in preeclampsia incidence when aspirin is started before 16 weeks.
Nutrition‑Based Prevention: The Unsung Hero
While not a medication, proper nutrition underpins all prophylactic efforts. Regular intake of prenatal vitamins containing folic acid, iodine, and iron reduces neural‑tube defects and anemia. Food safety practices-cooking meat thoroughly, avoiding unpasteurized dairy, and washing produce-prevent listeriosis, toxoplasmosis, and salmonella.
How to Build Your Personal Prophylaxis Plan
- Schedule a pre‑conception or first‑trimester visit. Bring a list of any chronic conditions, medications, and upcoming travel plans.
- Review vaccination status. Your clinician will check for flu, Tdap, hepatitis B, COVID‑19, and any region‑specific vaccines.
- Discuss screening tests. GBS swab timing, chorionic villus sampling, and any genetic panels should be clarified.
- Plan medication safety. Identify antibiotics, antimalarials, or anticoagulants you may need, and confirm dosages.
- Set nutrition goals. Choose a prenatal vitamin with 400‑800 µg folic acid, 30 mg iron, and 150 µg iodine.
- Create a contingency plan. Know the nearest hospital with a maternal‑fetal medicine unit in case of emergency.
Document this plan in a printable sheet or a health‑app reminder. Consistency is key-missed doses or delayed vaccines can undermine protection.
Comparison of Common Prophylactic Measures in Pregnancy
| Measure | Target Condition | Ideal Timing | Recommended Dose / Regimen | Key Considerations |
|---|---|---|---|---|
| Influenza vaccine | Seasonal flu | Any trimester, before flu season | 0.5 mL intramuscular | Safe in all trimesters; repeat annually |
| Tdap vaccine | Pertussis (whooping cough) | 27‑36 weeks | 0.5 mL intramuscular | Boosts newborn immunity for first 2 months |
| GBS antibiotic prophylaxis | Group B Streptococcus sepsis | Intrapartum (once labor starts) | Penicillin G 5 million U IV every 4 h | Based on positive swab at 35‑37 weeks |
| Malaria prophylaxis (ACT + weekly chloroquine) | Plasmodium infection | Start 1‑2 weeks before travel, continue 4 weeks after return | Weight‑adjusted ACT regimen, then 300 mg chloroquine weekly | Avoid first trimester if possible; monitor liver function |
| Low‑dose aspirin | Preeclampsia prevention | Before 16 weeks, continue until 36 weeks | 81 mg orally daily | Contraindicated in bleeding disorders |
Common Myths About Pregnancy Prophylaxis
- Myth: Vaccines can cause miscarriage.
Fact: Extensive research (e.g., 2021 meta‑analysis of >1 million pregnancies) shows no link between recommended vaccines and pregnancy loss. - Myth: Antibiotics are unsafe for the baby.
Fact: Certain antibiotics (penicillin, cephalosporins) are classified as Category B and are routinely used during labor. - Myth: You only need vaccines if you’re high‑risk.
Fact: Universal recommendations exist because all pregnant women benefit from herd immunity and personal protection.
When to Seek Professional Help
If you experience any of the following, contact your obstetrician immediately:
- Fever >38 °C that doesn’t resolve with acetaminophen.
- Painful swelling or redness at a vaccination site lasting more than 48 hours.
- Signs of an allergic reaction (hives, difficulty breathing).
- Unexplained vaginal bleeding after receiving prophylactic medication.
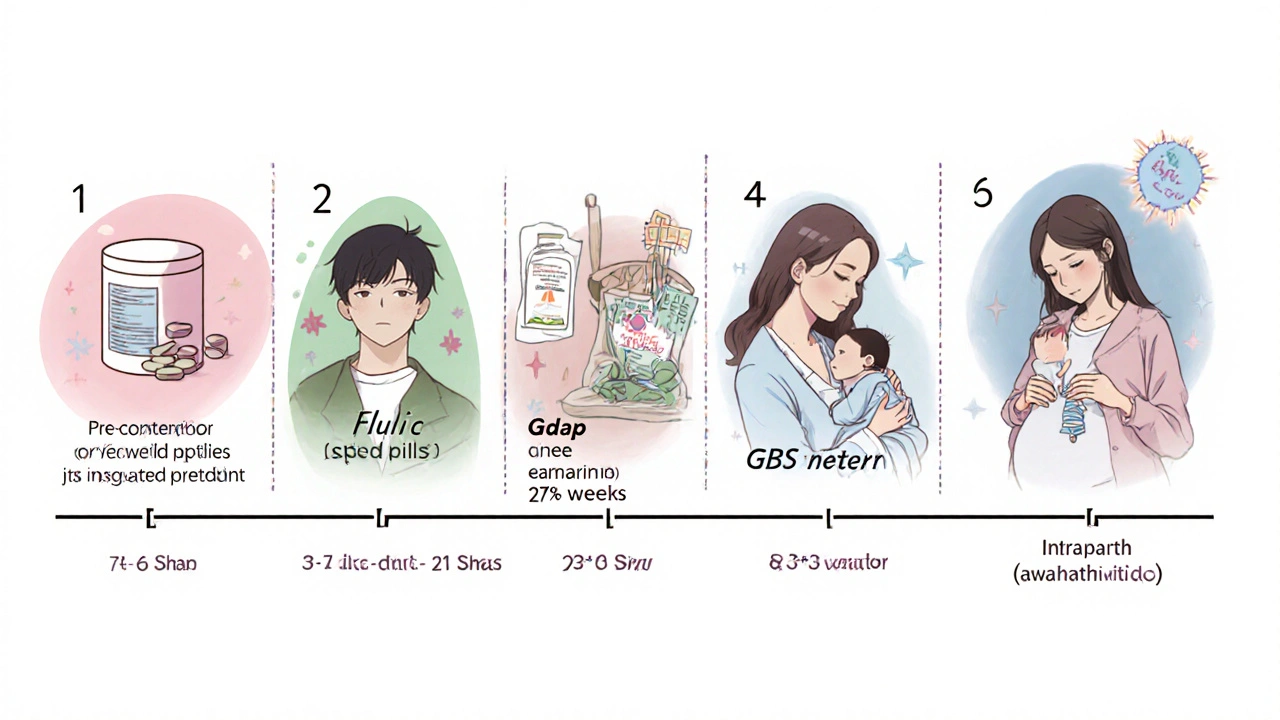
Putting It All Together: A Sample Timeline
| Gestational Age | Action |
|---|---|
| Pre‑conception / First visit | Check immunization records; start folic acid 400 µg daily. |
| 8‑12 weeks | Administer influenza vaccine if flu season is approaching. |
| 13‑16 weeks | Begin low‑dose aspirin for preeclampsia risk (if indicated). |
| 20‑24 weeks | Screen for anemia, repeat iron supplement if needed. |
| 27‑36 weeks | Give Tdap vaccine; schedule GBS swab at 35‑37 weeks. |
| Labor onset | If GBS positive, administer IV penicillin during labor. |
Key Takeaways
- Prophylaxis is a proactive, evidence‑based set of measures that protect both mother and baby.
- Vaccines (influenza, Tdap, hepatitis B, COVID‑19) are safe at any stage and should be timed strategically.
- Targeted antibiotics prevent neonatal infections like GBS when administered correctly.
- Travel to malaria‑endemic areas requires a tailored drug regimen and timing.
- Low‑dose aspirin and heparin can thwart clot‑related complications in high‑risk pregnancies.
- Combine medical interventions with sound nutrition and food safety for maximum protection.
Frequently Asked Questions
Is it safe to get the flu shot while pregnant?
Yes. The inactivated flu vaccine has been shown safe in all trimesters and protects both mother and baby from severe flu complications.
When should I receive the Tdap vaccine?
Ideal timing is between 27 and 36 weeks of gestation, allowing antibodies to cross the placenta and shield the newborn from pertussis.
Do I need antibiotics for a urinary tract infection during pregnancy?
Often yes. Certain safe antibiotics (e.g., nitrofurantoin, amoxicillin) are prescribed to treat UTIs and prevent kidney infections that could affect the pregnancy.
Can I travel to a malaria‑risk country while pregnant?
Travel is discouraged in the first trimester. If travel is unavoidable, a specialist will plan a prophylactic regimen using ACT followed by weekly chloroquine or mefloquine, depending on resistance patterns.
Should I take low‑dose aspirin even if I have no risk factors?
Current NICE guidelines advise aspirin only for women with identified risk factors (e.g., previous preeclampsia, chronic hypertension). Unnecessary use can increase bleeding risk.
Staying ahead with the right preventive steps lets you focus on the excitement of upcoming parenthood instead of worrying about avoidable health scares. Talk to your obstetrician, keep a written plan, and follow the schedule-your baby will thank you.

10 Responses
Reading this guide feels like stumbling upon a hidden manual that the mainstream medical establishment doesn't want you to see, because it reveals how covert alliances between pharmaceutical giants and government agencies shape the very recommendations we trust. The narrative around pregnancy prophylaxis is deliberately simplistic, designed to keep us compliant while the real agenda focuses on profit margins rather than genuine maternal health. While the article mentions flu shots and Tdap, it conveniently omits the decades‑long data on adjuvant‑induced autoimmunity that some independent studies have flagged. Moreover, the emphasis on low‑dose aspirin glosses over the fact that aspirin manufacturers fund a large portion of the cited research, creating a conflict of interest that is rarely disclosed. The guide also praises malaria prophylaxis with ACT regimens, but fails to discuss how certain ACT components are patent‑locked, ensuring that low‑income countries remain dependent on expensive imports. Nutrition‑based prevention is presented as a benign lifestyle choice, yet the supplement industry capitalizes on pregnant women's anxieties, pushing multi‑vitamin packages that are often overpriced and contain redundant nutrients. There is a deeper layer here: every recommendation subtly nudges pregnant women toward a cycle of medicalization that funnels billions into the healthcare economy. The schedule of vaccines appears orderly, but the timing aligns perfectly with the roll‑out schedules of new vaccine batches, raising eyebrows about synchronicity. While the guide applauds GBS screening, it ignores the emerging data suggesting that over‑use of intrapartum antibiotics may contribute to rising neonatal microbiome disturbances. The mention of COVID‑19 vaccines is framed as universally safe, yet it sidesteps the ongoing debates about myocarditis risk in younger populations, a topic that mainstream outlets routinely downplay. Even the travel prophylaxis advice is calibrated to promote the use of branded antimalarial drugs, marginalizing affordable generic alternatives that could be equally effective. In short, the article is a masterclass in selective disclosure, offering just enough evidence to appear credible while shielding the reader from the full spectrum of controversies and vested interests that underlie each recommendation.
The guide does a solid job breaking down the why and when of each vaccine, especially for first‑time moms who can feel overwhelmed by medical jargon. I appreciate how it stresses the safety of the flu shot across all trimesters – that’s a game‑changer for moms worrying about catching something serious. Also, the clear timeline for Tdap really helps schedule appointments without last‑minute scrambling.
Love the upbeat vibe! Knowing that low‑dose aspirin can cut preeclampsia risk by 30% makes me feel empowered to take proactive steps. The nutrition tips are spot on – I’ve already added a prenatal vitamin with 800 µg folic acid to my routine.
While the article is thorough it omits the philosophical dimension of trust in medical authority – a discourse often ignored. One could argue that prophylaxis isn’t merely clinical but an existential negotiation between body and society.
From a pathophysiological perspective, the guide could benefit from delineating the mechanistic pathways by which Tdap‑induced IgG transplacental transfer attenuates neonatal pertussis morbidity. Moreover, integrating pharmacokinetic parameters for low‑dose aspirin would enhance clinical applicability.
It’s heartbreaking how many expectant mothers feel abandoned by the system – this guide is a beacon, but the real world often feels like a cold, endless night.
For those seeking to implement this plan, I recommend creating a shared digital document with your obstetrician, listing each prophylactic measure, its scheduled timing, and any required follow‑up labs. This structured approach ensures accountability and facilitates seamless communication across care teams.
Hey everyone, just a heads up – if you’re traveling soon, double‑check the ACT dosage chart with your pharmacist. It saved me a ton of stress last month!
Always discuss medication changes with your provider.
Philosophically, prophylaxis reflects an inherent tension between determinism and agency – we are urged to preempt fate, yet the very act of prevention reshapes the narrative of prenatal care. Aggressively confronting misinformation is essential; silence only fortifies falsehoods. Let’s champion evidence while demanding transparency from all stakeholders.