Peripheral artery disease, or PAD, isn’t just about sore legs after walking. It’s a warning sign your whole body is at risk. When arteries in your legs, arms, or other extremities narrow from plaque buildup, your muscles don’t get enough blood-especially when you’re active. This isn’t normal aging. It’s a serious condition that affects 8.5 million Americans, mostly over 65. And if you have PAD, your chances of having a heart attack or stroke jump by 3 to 5 times. Most people don’t know they have it until something serious happens. But catching it early can save your limbs-and your life.
What Does PAD Actually Feel Like?
The classic symptom is claudication: pain, cramping, or tiredness in your calves, thighs, or hips that shows up when you walk or climb stairs-and disappears after a few minutes of rest. It’s not just being out of shape. It’s your muscles screaming for oxygen they can’t get because blood flow is blocked.
But not everyone feels this. About 40% of people with PAD have no symptoms at all. That’s why it’s called a silent threat. Others notice more subtle signs: cold feet, shiny skin on the lower legs, loss of leg hair, or toenails that grow slow and thick. Men might experience erectile dysfunction-it’s not just a sexual issue, it’s a vascular one. When arteries in the pelvis narrow, it affects blood flow everywhere.
In the worst cases, you get rest pain. That means your toes or feet hurt even when you’re lying down. You might find yourself hanging your foot off the bed at night just to get relief. Or you notice a sore on your foot that won’t heal, no matter how long you wait. This is critical limb ischemia-the most dangerous stage. Without treatment, gangrene can set in, and amputation becomes a real possibility.
How Do Doctors Diagnose PAD?
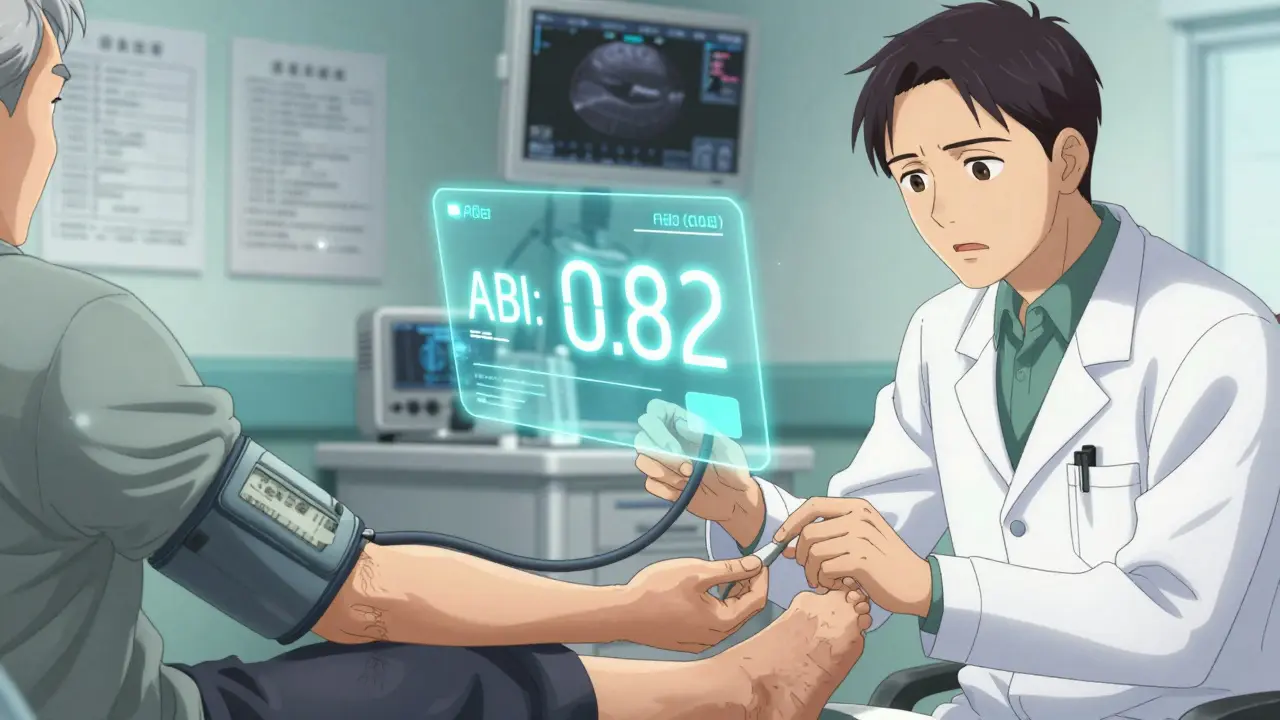
Diagnosing PAD starts with a simple test called the ankle-brachial index, or ABI. It’s non-invasive, quick, and costs less than $20. Your doctor measures your blood pressure at your arm and your ankle, then compares the two. If the ankle pressure is less than 90% of the arm pressure (ABI ≤ 0.90), you have PAD. This test catches 95% of cases accurately.
But if you have diabetes or kidney disease, your arteries might be stiff and hard to compress. In those cases, doctors use the toe-brachial index (TBI). A TBI under 0.70 means trouble. Doppler ultrasound is the next step-it shows exactly where the blockage is and how fast blood is flowing. It’s like a real-time video of your arteries.
For more detail, doctors may order a CT angiogram or an MRI angiogram. These create 3D images of your blood vessels. They’re not always needed, but if surgery is being considered, they give surgeons a clear map. Catheter angiography is the most accurate-it’s the gold standard-but it’s invasive. It involves threading a thin tube into your artery and injecting dye. It’s reserved for cases where intervention is likely.
Screening isn’t routine for everyone. But the American Heart Association says you should get tested if you’re:
- 65 or older
- 50 or older with diabetes or a history of smoking
- 40 or older with multiple risk factors like high blood pressure, high cholesterol, or obesity
Yet only about 20% of eligible people get screened. That’s a huge gap. If you’re in one of these groups and have even mild leg discomfort, ask for an ABI test. It could change everything.
Lifestyle Changes Are the First Line of Defense
Medication helps-but nothing beats changing your habits. The most powerful treatment for PAD isn’t a pill. It’s walking.
Supervised exercise therapy means walking on a treadmill or track under guidance, three to five times a week, for 30 to 45 minutes. You walk until you feel pain, rest until it goes away, then keep going. After 12 weeks, most people can walk 150% to 200% farther without pain. That’s not magic. It’s your body building new tiny blood vessels to bypass the blockages.
Quitting smoking is non-negotiable. If you keep smoking, your risk of amputation goes up by 8 times. Your chance of dying within five years jumps by 300%. That’s not a scare tactic. That’s data from the Mayo Clinic. Nicotine damages blood vessels, makes clots more likely, and slows healing. If you quit, your risk drops dramatically-even if you’ve smoked for 40 years.
Diet matters too. Cutting back on saturated fats and sugars helps lower LDL cholesterol. And you need to get that number under 70 mg/dL. That’s the target for PAD patients, even if your cholesterol was normal before.
Medications That Actually Work
There are three key drugs for PAD:
- Antiplatelets: Aspirin (81 mg daily) or clopidogrel (75 mg daily). Clopidogrel is slightly better at preventing heart attacks and strokes. The CAPRIE trial showed a 20.5% lower risk with clopidogrel compared to aspirin.
- Statins: Atorvastatin, rosuvastatin, or simvastatin. These aren’t just for cholesterol. They stabilize plaque, reduce inflammation, and cut cardiovascular events by 25-30%. The ACC/AHA says ALL PAD patients need a high-intensity statin, no matter their starting number.
- Cilostazol: This drug helps you walk farther by improving blood flow and reducing clotting. It can increase pain-free walking distance by 50-100%. But it’s not for everyone-don’t take it if you have heart failure.
Some patients get blood thinners like rivaroxaban (2.5 mg twice daily) along with aspirin. The VOYAGER PAD trial showed this combo reduces the risk of limb complications and heart events by 15% in people who’ve had a procedure. It’s not for everyone, but it’s a game-changer for high-risk cases.
When Procedures Are Needed
If walking and pills aren’t enough, and your pain is stopping you from living, it’s time to think about procedures.
Balloon angioplasty is the most common. A tiny balloon is inserted into the blocked artery and inflated to open it up. It works well for short blockages-success rates hit 90%. Sometimes a stent (a metal mesh tube) is left behind to keep the artery open. One-year patency rates are around 80% for arteries in the thigh.
Atherectomy removes plaque mechanically. It’s useful when the blockage is hard and calcified-common in diabetics. Success rates are about 75%.
Bypass surgery is the most invasive. A surgeon uses a vein from your leg or a synthetic graft to reroute blood around the blocked section. It’s durable-80% of vein bypasses stay open after five years. But recovery takes weeks, and it’s not for frail patients.
The BASIL trial found that for people with claudication, doing exercise alone gives the same long-term results as doing a procedure plus exercise. But if you’re in pain and can’t walk, the procedure gets you back on your feet faster. The choice depends on your goals, your health, and your lifestyle.

What Happens If You Don’t Treat It?
PAD doesn’t get better on its own. Left untreated, it can lead to:
- Chronic wounds that never heal
- Severe infections in the foot or leg
- Tissue death (gangrene)
- Amputation
And it doesn’t stop at your legs. PAD is a sign your heart and brain arteries are probably clogged too. The five-year death rate for PAD patients is 30-40%. That’s higher than many cancers. You’re not just at risk for a bad leg-you’re at risk for a fatal heart attack or stroke.
That’s why treating PAD isn’t optional. It’s survival.
What’s New in PAD Care?
Research is moving fast. The PAD Awareness Act of 2022 gave $5 million a year to fund free screening programs for high-risk groups. That’s a big step toward catching more cases early.
Stem cell therapy is being tested for critical limb ischemia. In early trials, injecting a patient’s own CD34+ stem cells into the leg improved wound healing in 65% of cases-compared to just 35% in those who didn’t get the treatment. It’s still experimental, but promising.
New imaging tools like optical coherence tomography (OCT) let doctors see plaque in incredible detail-down to the microscopic level. This helps them choose the best treatment, whether it’s a stent, a drug-coated balloon, or something else.
But the biggest barrier isn’t technology. It’s awareness. Black and Hispanic patients are 30-40% less likely to get revascularization procedures-even when their disease is just as severe. Access to care still varies too much by race, income, and location.
What Should You Do Now?
If you’re over 50 and smoke, or you have diabetes, or you’ve noticed leg pain when walking, don’t wait. Ask your doctor for an ABI test. It takes five minutes. No needles. No radiation. Just two blood pressure cuffs.
If you’re diagnosed, don’t panic. You have options. Start walking. Quit smoking. Take your meds. Work with a vascular specialist. You don’t have to lose your leg. You don’t have to die early. PAD is treatable. But only if you act.
The sooner you start, the better your chances. Your legs aren’t just for walking-they’re your lifeline to a longer, healthier life.
Can peripheral artery disease be reversed?
Yes, in many cases. While damaged arteries won’t fully return to normal, plaque can stabilize and shrink with aggressive treatment. Lifestyle changes-especially walking, quitting smoking, and taking statins-can improve blood flow enough to eliminate symptoms. Some patients go from needing a cane to walking miles without pain. The key is consistency. It’s not about a miracle cure-it’s about daily habits that rebuild your vascular health over time.
Is PAD the same as varicose veins?
No. Varicose veins are swollen, twisted surface veins caused by faulty valves. They’re mostly a cosmetic issue or cause mild discomfort. PAD is about blocked arteries deep in the legs, cutting off oxygen to muscles. It causes pain during activity, not just swelling or heaviness. One affects veins, the other arteries. One is often harmless; the other can be life-threatening.
Why does PAD cause erectile dysfunction?
Erectile dysfunction happens when blood flow to the penis is restricted. The arteries there are small and sensitive to plaque buildup. If those arteries are narrowed, it’s a strong signal that larger arteries-like those in the heart and legs-are also affected. In fact, 45-75% of men with PAD also have ED. It’s often one of the earliest signs of vascular disease, sometimes appearing years before leg pain.
Can I still exercise if I have PAD?
Yes-and you should. Walking is the most effective treatment. Start slow. Walk until you feel moderate pain, stop and rest until it fades, then walk again. Repeat. This trains your body to create new blood vessels around the blockages. Many patients find they can walk farther without pain after just 12 weeks. Avoid sitting still for long periods. Movement is medicine.
What’s the difference between ABI and TBI?
ABI measures blood pressure in the ankle compared to the arm. TBI does the same but uses the big toe instead of the ankle. TBI is used when ankle arteries are too stiff to compress-common in people with diabetes or kidney disease. A TBI below 0.70 indicates PAD. Both tests are accurate, but TBI is more reliable when standard ABI results are unclear.
Does PAD increase the risk of heart attack?
Yes, significantly. PAD means atherosclerosis is affecting your entire body-not just your legs. People with PAD have a 3 to 5 times higher risk of heart attack or stroke than those without it. That’s why treatment focuses not just on leg symptoms, but on protecting your heart and brain. Statins, blood pressure control, and antiplatelet drugs are all aimed at reducing that overall risk.
How long does it take to see results from PAD treatment?
It varies. Walking programs show improvement in 6 to 12 weeks. Medications like statins and antiplatelets work over months to reduce long-term risk. Smoking cessation has immediate benefits-blood flow improves within weeks. Procedures like angioplasty can relieve pain almost instantly. But lasting results require ongoing commitment. PAD management is a lifelong effort, not a quick fix.
Are there any natural remedies for PAD?
There’s no proven natural cure. Supplements like ginkgo biloba or L-arginine have been studied but show no consistent benefit. The only natural treatment with strong evidence is exercise. Eating a heart-healthy diet (low in salt, sugar, and saturated fat) helps. But don’t replace proven medical treatments with herbs or vitamins. They won’t stop a heart attack or save your leg.
If you’re living with leg pain, cold feet, or non-healing sores, don’t ignore it. PAD is common, treatable, and often silent. The tools to diagnose and manage it exist. What’s missing is awareness. Take the first step: ask your doctor for an ABI test. Your future self will thank you.


11 Responses
Man, I never realized PAD was this insidious. The ABI test sounds like a no-brainer-five minutes, no needles, and it could literally save your leg. I’m getting mine next week. My dad had silent PAD and lost a toe before they caught it. Don’t wait for the pain to be unbearable.
Also, the statin point? Non-negotiable. My vascular doc said if your LDL isn’t under 70, you’re just delaying the inevitable. No more ‘it’s fine’ nonsense.
Let’s be real-this isn’t just about legs. PAD is your body’s red alert that your entire vascular system is on fire. And yet, so many people dismiss calf cramps as ‘getting old’ or ‘not being fit.’ It’s not. It’s atherosclerosis screaming for attention. The fact that 40% of cases are asymptomatic is terrifying. We need mass screening campaigns, not just pamphlets in waiting rooms. Insurance companies should cover ABI for anyone over 50 with any risk factor-period. This isn’t elective healthcare. It’s preventative survival.
And yes, walking works. Not because it’s trendy, but because it triggers angiogenesis. Your body builds new highways when the old ones are blocked. It’s biological ingenuity. You don’t need a gym. You need a sidewalk, a timer, and the will to walk through pain. Consistency beats intensity every time.
Quit smoking. That’s it. That’s the whole post. Everything else is just noise. If you’re smoking and have PAD, you’re playing Russian roulette with your limbs. No magic pill, no fancy procedure, no supplement will fix what nicotine destroys. I’ve seen it. I’ve had patients walk in with blackened toes and still say ‘I’ll quit after the amputation.’ No. Just… no.
Start walking. Take your statin. Get the test. But if you don’t quit smoking, none of it matters. You’re just buying time with a ticking clock.
I love how this post doesn’t just list facts-it tells a story. The part about hanging your foot off the bed at night? That’s the kind of detail that sticks with you. I’ve got an uncle who ignored his cold feet for years. Thought it was just ‘bad circulation.’ Then he got a sore that wouldn’t heal. By the time he went in, they were talking amputation. He’s on a walker now, but he’s alive because he finally listened.
Also, the ED-PAD link? That’s something men need to hear. It’s not embarrassing-it’s diagnostic. If you’ve got ED and you’re over 50, get your ABI checked. It’s not about sex. It’s about survival.
It is indeed a matter of grave concern that peripheral artery disease remains underdiagnosed in many communities, particularly in regions with limited access to vascular screening. In Nigeria, where cardiovascular diseases are rising rapidly, awareness remains minimal. The ABI test, being inexpensive and non-invasive, should be integrated into primary care protocols across the continent. We must not wait for limb loss before acting. Prevention through education and accessible diagnostics is not a luxury-it is a moral imperative.
Pad is real. I seen guy in my village, 62, smoked 40 years, no pain till one day foot turn black. Now he got prosthetic. Doc said if he did walking 30 min a day, he coulda kept leg. But he didn’t. Now he cant even go to temple. Sad.
i wonder if the real issue isnt pad but the pharmaceutical industry pushing drugs like cilostazol and rivaroxaban because they make more money than telling people to just walk and stop smoking. like why do we need a $2000 stent when a $0 walk works better? maybe the system is designed to keep us sick. also, why is the american heart association so involved? are they funded by big pharma? just sayin.
As a public health professional, I commend this comprehensive overview. The emphasis on supervised exercise therapy is critical-especially in low-resource settings where medication access is limited. In India, we’ve piloted community-based walking groups for PAD patients with remarkable adherence. Local health workers, trained in basic ABI measurement, can bridge the diagnostic gap. We must decentralize care. No one should die because they live too far from a vascular specialist. Policy must follow science: free ABI screenings in primary centers, smoking cessation programs in every rural clinic, and statins as essential medicine. This is not just medicine-it’s justice.
They’re lying about PAD being caused by plaque. It’s actually caused by 5G radiation and fluoride in the water. The doctors are paid by the amputation industry to scare you into getting unnecessary procedures. Your leg doesn’t need a stent-it needs detoxing and a Faraday cage. I’ve been researching this for 12 years. The ABI test? It’s calibrated to lie. I tested myself with a ruler and a watch. My ‘ABI’ was 1.5. They told me I had severe PAD. I told them to shove their ultrasound.
Just had my first ABI test last week-turns out I had borderline PAD. Started walking 20 mins a day. Two weeks in, I can go up and down stairs without gasping. It’s not magic. It’s biology. Also, I quit smoking cold turkey after reading this. No patches. No vaping. Just said ‘no.’ My feet feel warmer already. If you’re reading this and you’re scared? Start walking today. Not tomorrow. Today.
And if you think you’re too old? You’re not. My 78-year-old neighbor walks 3 miles every morning. He’s got PAD. And he’s still hiking in the Rockies. You can too.
ABI test. Now. If you’re over 50 and ever smoked. No excuses.