What is neuropathic pain?
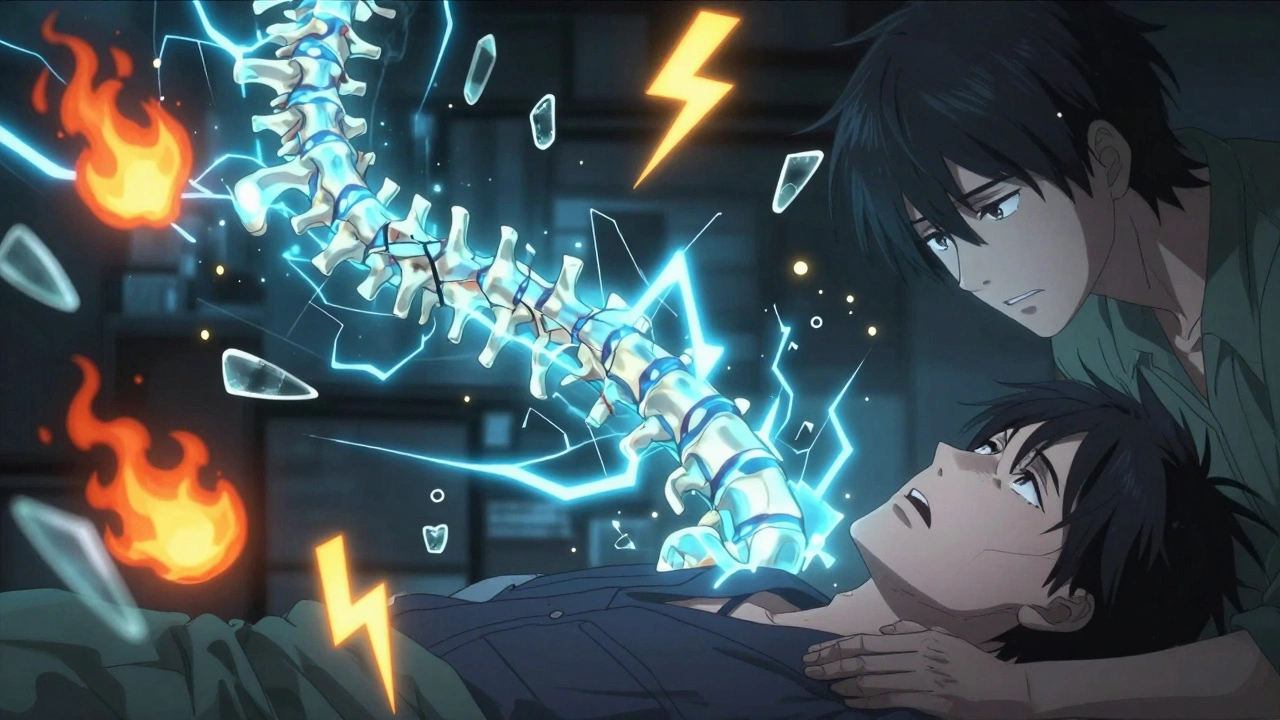
Neuropathic pain isn't the kind of pain you feel when you stub your toe or pull a muscle. It comes from damaged or malfunctioning nerves. Think of it like a faulty electrical wire in your body-instead of sending normal signals, it fires off random, painful bursts. People describe it as burning, shooting, or like electric shocks. Some feel tingling, numbness, or even pain from something light brushing against their skin, like a bedsheet. This isn’t just discomfort-it’s often constant, disruptive, and doesn’t respond to regular painkillers like ibuprofen or acetaminophen.
About 7 to 10% of adults deal with this kind of pain. Diabetes is the biggest cause, accounting for roughly 30% of cases. Other common triggers include shingles, spinal injuries, surgeries, chemotherapy, and vitamin B12 deficiency. The International Association for the Study of Pain officially defined it in 2022, and since then, treatment guidelines have evolved to focus on both treating the root cause and managing the pain itself.
Why gabapentin and pregabalin are first-line treatments
For decades, doctors turned to opioids for chronic pain. But with addiction risks and limited long-term benefits, guidelines shifted. Today, gabapentin and pregabalin are the go-to medications for neuropathic pain. Both were originally designed as anti-seizure drugs but were found to calm overactive nerves. They work by targeting the alpha-2-delta subunit of calcium channels in the spinal cord and brain. This reduces the release of pain-signaling chemicals like glutamate and substance P.
The American Academy of Neurology and the Neuropathic Pain Special Interest Group (NeuPSIG) both list them as first-line options. Around 60% of people with neuropathic pain are prescribed one of these two. Neither is addictive like opioids, and they don’t cause liver damage like some other pain meds. But they’re not magic pills-they help about one in three people get at least half their pain relief. That’s not perfect, but for many, it’s life-changing.
Gabapentin: How it works and what to expect
Gabapentin, sold under brand names like Neurontin, has been around since the 1990s. It’s available as capsules, tablets, and extended-release versions. The usual starting dose is 100 to 300 mg at night, slowly increasing over weeks. Most people end up taking 900 to 3,600 mg daily, split into three doses because it leaves the body quickly-half gone in just 5 to 7 hours.
That’s the catch: dosing is messy. You have to take it three times a day, and if you miss a dose, the pain can come back fast. Many patients give up because it’s hard to stick to. A 2023 JAMA study found 34.7% of people quit gabapentin within the first few months, mostly because of the complex schedule.
Side effects are common but usually mild: dizziness (about 26% of users), sleepiness (19%), swelling in the legs (10%), and feeling unsteady on your feet. It’s not great for older adults or people with kidney problems. Dose adjustments are needed if your kidneys aren’t working well. On the plus side, it’s cheap. Generic gabapentin costs about $16 for a 90-day supply of 300 mg capsules. It doesn’t cause weight gain in most people-only 3% report it.
Pregabalin: Faster, stronger, but costlier
Pregabalin, known as Lyrica, is the newer sibling. It works the same way as gabapentin but binds to the nerve target six times more tightly. That means it’s more powerful. You need less of it. A typical dose is 75 to 150 mg twice a day, with a maximum of 600 mg daily. It’s absorbed fully, no matter what you eat, and stays in your system longer-6.3 hours on average. That makes twice-daily dosing easy.
Because of this, patients reach effective doses faster. In one 2023 trial, people on pregabalin hit their target dose in under 8 days. Gabapentin took nearly 15. That’s why many doctors prefer it for people who struggle with daily routines.
But there’s a trade-off. Pregabalin causes more weight gain-about 12% of users gain 5 to 15 pounds in the first month. Dizziness and sleepiness are also more common than with gabapentin. And it’s expensive. Even generic versions cost around $28 for 60 capsules of 75 mg. That’s nearly double the price of gabapentin.
Because of its higher abuse potential, pregabalin is now a Schedule V controlled substance in the U.S. That means prescriptions are tracked, refills are limited, and some pharmacies require extra paperwork. In 2023, there were 12.3 overdose deaths linked to pregabalin. Gabapentin? Zero.
Head-to-head: Which one works better?
Direct comparisons show pregabalin has a slight edge in effectiveness. In a 2021 meta-analysis of over 4,000 patients, 300 mg of pregabalin gave the same pain relief as 3,600 mg of gabapentin. Another study found 68% of pregabalin users reached 50% pain reduction at 12 weeks, compared to 59% for gabapentin.
But real-world results are mixed. A 2024 analysis of 3,842 patients on PatientsLikeMe showed pregabalin scored higher for effectiveness (6.2/10) but lower for tolerability (4.8/10). Gabapentin scored lower on pain relief (5.7/10) but higher on tolerability (5.9/10).
Reddit threads tell the same story. One user wrote: “Pregabalin cut my pain from 8 to 3 in two days-but I gained 12 pounds.” Another said: “Gabapentin made me dizzy and fall twice. Switched to pregabalin-no dizziness, same relief.”
For diabetic neuropathy, the American Diabetes Association recommends pregabalin first. For people on tight budgets or with kidney issues, gabapentin still holds value. And for those who can’t handle weight gain or sedation, gabapentin might be the better pick-even if it takes longer to work.
Who should take which?
There’s no one-size-fits-all answer. But here’s how most doctors decide:
- Choose pregabalin if: You need fast results, have trouble remembering multiple daily doses, or are in a setting where cost isn’t a barrier (like a private clinic or academic hospital). It’s also preferred if you have diabetic neuropathy.
- Choose gabapentin if: Cost is a major concern, you’re worried about weight gain, or you’re being treated in a safety-net clinic or rural area. It’s also safer for people with mild kidney problems if doses are adjusted properly.
Some patients start with gabapentin to test tolerance. If side effects are too bad or it doesn’t help enough after 6 weeks, they switch to pregabalin. Others start with pregabalin and drop down to gabapentin if weight gain becomes an issue.
Both medications require slow titration. Jumping to a high dose increases side effects without better pain relief. Most doctors recommend starting low and going slow-especially for older adults.
What about side effects and risks?
Both drugs come with warnings. In 2008, the FDA added black box labels for both, highlighting rare but serious risks like suicidal thoughts and angioedema (swelling of the face or throat). These are uncommon-about 0.4% for suicidal ideation, 0.08% for swelling-but you need to watch for them.
Don’t stop either drug suddenly. That can trigger seizures, even in people who’ve never had them. Tapering down over weeks is essential.
Other risks: Both can cause dizziness and drowsiness, which increases fall risk in older adults. Avoid alcohol. Don’t drive or operate heavy machinery until you know how it affects you.
Drug interactions are minimal with gabapentin. Pregabalin can interact with blood pressure meds and opioids, making drowsiness worse. Always tell your doctor what else you’re taking.
What’s next for neuropathic pain treatment?
Neither gabapentin nor pregabalin is perfect. Newer drugs like duloxetine (an SNRI) and venlafaxine are gaining ground, especially for diabetic neuropathy. In 2024, the FDA approved a once-daily extended-release version of pregabalin (Lyrica CR), which may improve adherence. Gabapentin enacarbil (Horizant) is also being used more for restless legs syndrome.
But experts agree: these two drugs aren’t going away anytime soon. Gabapentin will stay popular because it’s cheap and widely available. Pregabalin will slowly lose market share as newer options arrive, but it’ll remain a key tool for those who need fast, reliable relief.
The future of neuropathic pain management is multimodal-combining meds with physical therapy, nerve blocks, cognitive behavioral therapy, and lifestyle changes. Medications alone rarely fix everything. But for millions, gabapentin or pregabalin is the first step back to a normal life.
When to see a specialist
If you’ve been on gabapentin or pregabalin for 6 to 8 weeks at the highest tolerated dose and your pain hasn’t improved by at least 30%, it’s time to see a pain specialist. Primary care doctors often struggle with dosing these drugs. Pain clinics can fine-tune treatment faster-some get patients to optimal doses in under a week, compared to over 11 days in general practice.
Also, if you’re experiencing new symptoms like muscle weakness, numbness spreading to other areas, or loss of bladder control, don’t wait. These could signal something else-like spinal stenosis or multiple sclerosis-that needs different treatment.

11 Responses
I've been on gabapentin for 3 years for diabetic neuropathy. It's not perfect but it lets me sleep. Dizziness? Yeah. But I'd rather be dizzy than screaming at 3am. My cat even knows when I'm about to take it - she sits on my lap like she's guarding me.
I used to think these meds were just placebo until my mom stopped crying every night after starting pregabalin. She went from hiding under blankets to gardening again. Not magic. But close enough. The weight gain sucked but we traded it for peace. Sometimes that’s the only win you get.
In India, gabapentin is available over the counter in many places. No prescription needed. People take it for anxiety, insomnia, even headaches. The lack of regulation here is dangerous. I’ve seen people on 6000mg a day with zero medical supervision. It’s not a supplement.
Pregabalin is just Big Pharma’s fancy version of gabapentin. They just repackaged the same drug and slapped a $200 price tag on it. And now they’re calling it ‘controlled’? Please. The only thing controlled here is your wallet.
The 2024 PatientsLikeMe data is misleading. The sample is self-selected - people who are active online and have strong opinions. Those who tolerated gabapentin well rarely post. Those who gained 15 pounds and felt like a zombie? They’re the ones flooding Reddit. Real-world adherence studies show similar efficacy when dosed properly.
I’m from the Midwest. We don’t get fancy meds here. Gabapentin is all we’ve got. My doctor doesn’t even know what pregabalin is. And honestly? I don’t care. It works. I take it with coffee. I don’t fall over. I don’t gain weight. I live. That’s enough.
I’ve been on both. Gabapentin made me feel like a zombie who forgot how to blink. Pregabalin? Made me cry for no reason and gain 20 pounds in 6 weeks. I’m not even mad. I’m just… tired. Why does everything that helps you feel better also destroy your body? Why can’t medicine just be simple?
I’m from Mumbai. My cousin took gabapentin for post-chemo pain. He’s a truck driver. Three times a day? Impossible. He missed doses, pain came back, he got fired. Then they switched him to pregabalin - twice a day. He’s back on the road. Cost? We paid out of pocket. Worth it. No one should lose their job because of a dosing schedule.
Let’s be real - these drugs are just sedatives with a fancy label. They don’t fix the nerve damage. They just make you too tired to care. And now we’re calling them ‘first-line’? What about real solutions? Physical therapy? Acupuncture? Or maybe… stop making people take pills for life because we won’t fix the root cause?
My doc started me on gabapentin. I got dizzy. Switched to pregabalin. Gained weight. Switched to duloxetine. Now I’m on a combo. Pain’s at a 4 instead of 8. Not cured. But I can hold my kid again. That’s the goal. Not perfection. Just… more days like this.
Gabapentin is literally just a cheaper version of pregabalin. Stop pretending they’re different. It’s the same molecule with a bad delivery system. And if you’re still on gabapentin because it’s cheap, you’re being exploited. Your doctor’s not saving you money - they’re cutting corners.