Metronidazole Dose Tracker
Track your metronidazole dose to identify risk of peripheral neuropathy. The critical threshold is 42 grams. Exceeding this amount significantly increases your risk of nerve damage that can become permanent.
What to Do Next
Warning: If your total dose exceeds 42 grams, stop taking metronidazole immediately and consult your doctor.
Symptoms of neuropathy include:
- Tingling or numbness in hands and feet (often starting in the toes)
- Burning sensations
- Electric shock-like feelings
- Symmetrical symptoms spreading upward (stocking-glove distribution)
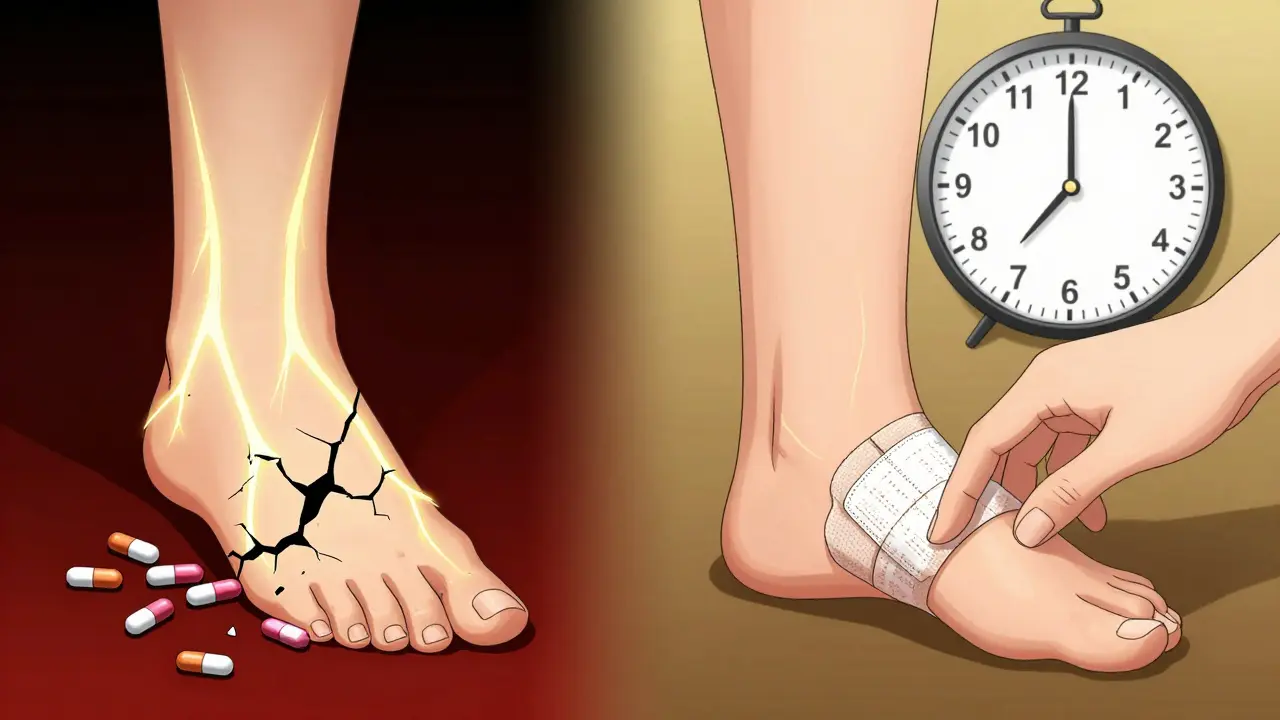
When you take metronidazole for a stubborn infection-whether it’s bacterial vaginosis, a C. diff flare-up, or a liver abscess-you expect relief, not new problems. But for some people, the very drug meant to kill bacteria starts attacking nerves instead. The signs are subtle at first: a pins-and-needles feeling in the toes, a dull numbness creeping up the feet, or sudden electric shocks in the hands. These aren’t random quirks. They’re warning signs of metronidazole neuropathy, a serious but often missed side effect that can turn temporary discomfort into permanent disability if ignored.
What Metronidazole Neuropathy Actually Feels Like
Metronidazole-induced peripheral neuropathy doesn’t hit all at once. It creeps in. Most people notice it in their feet first-like wearing socks that are too tight, even when they’re barefoot. The numbness isn’t just dull; it’s persistent. Tingling turns into burning. Some describe it as walking on broken glass. Others feel their feet are asleep all day, even after waking up. The symptoms usually spread symmetrically, moving from the feet upward toward the calves, and sometimes into the hands-a pattern doctors call a "stocking-glove" distribution.
It’s worse at night. Many patients report lying awake because the burning feels more intense when they’re still. Some can’t sleep because their feet feel like they’re on fire. One 69-year-old woman, treated for diverticulitis with 55 grams of metronidazole, said her pain was so severe she stopped walking altogether. Gabapentin helped a little, but not enough. Another man, a carpenter, lost his ability to grip tools because his fingers started feeling like they were full of static electricity.
This isn’t just about sensation. Some people develop autonomic symptoms-things like trouble regulating body temperature. A 15-year-old girl in a Duke University case study had to soak her legs in ice water just to ease the pain. That’s not normal. That’s your nervous system screaming for help.
How Much Is Too Much? The 42-Gram Threshold
Metronidazole is safe for short courses. A typical 7-day treatment for bacterial vaginosis? No problem. But when you take it for weeks or months-especially for chronic infections like recurrent C. diff or hepatic abscesses-the risk climbs fast. The tipping point? 42 grams total.
That’s not a lot. If you’re taking 500 mg three times a day, you hit 42 grams in about four weeks. Studies show that people who exceed this amount are more than 10 times more likely to develop neuropathy than those who stay under it. One patient received 168 grams over several months for a liver abscess. Another got 315 grams-nearly eight times the danger threshold. Both developed severe nerve damage.
Even worse, some cases have shown up after just 10 days of high-dose therapy. There’s no safe "long-term" dose. The longer you’re on it, the higher the risk. And because metronidazole is often prescribed as a last-resort antibiotic, patients end up on it longer than doctors realize.
Why This Happens: The Science Behind the Nerve Damage
Metronidazole doesn’t just kill bacteria-it crosses into your nerves. Once inside, its chemical structure breaks down into reactive molecules that attack nerve cells. Think of it like rust forming inside a wire. The nerves swell, the protective coating (myelin) breaks down, and signals start to misfire. That’s what causes the tingling, numbness, and pain.
Studies using nerve conduction tests show clear damage: reduced sensory signals, slower nerve responses, and signs of axonal degeneration. This isn’t just irritation-it’s structural damage. And unlike some drug side effects that fade quickly, this one can stick around even after you stop taking the drug.
It’s not random. The damage is dose-dependent and cumulative. Every extra pill adds up. That’s why doctors need to track total exposure, not just daily dosage.
Why It’s So Often Missed
Most doctors don’t think metronidazole causes nerve damage. In a 2023 survey, only 38% of primary care physicians knew the 42-gram risk threshold. Patients with diabetes get labeled as having "diabetic neuropathy"-even if they’ve never had high blood sugar. Elderly patients get written off as having "normal aging."
One Reddit user shared how he spent six months being told his numb feet were from sciatica, until he finally asked his pharmacist about metronidazole. That’s when the diagnosis clicked. He’d been on it for 12 weeks for C. diff prophylaxis. By then, the damage was done.
The problem is compounded by the fact that metronidazole’s common side effects-metallic taste, nausea, dizziness-are more obvious and get all the attention. The subtle nerve symptoms? They fly under the radar. But they’re the ones that can change your life.

How to Spot It Before It’s Too Late
You don’t need an MRI or a blood test to catch this early. Just ask yourself three questions:
- Have I been taking metronidazole for more than 4 weeks?
- Do I have numbness, tingling, or burning in my hands or feet?
- Are these symptoms worse at night or after standing for long periods?
If you answer yes to all three, stop the drug immediately and see a neurologist. Don’t wait for the symptoms to get worse. Don’t assume it’s "just a side effect."
Doctors can confirm it with an EMG (electromyography), which measures nerve function. But waiting for test results can cost you time-and nerve tissue. If your symptoms match the pattern and you’ve taken more than 42 grams, discontinuing metronidazole is the first and most critical step.
Recovery: How Long Does It Take?
Good news: most people get better. About 94% of patients see improvement or full recovery after stopping the drug. But "better" doesn’t mean fast.
Some notice relief in 2-4 weeks. Others take 3-6 months. The 15-year-old girl from Duke took six months to regain normal nerve function. One patient’s EMG showed complete recovery after 8 months. But recovery isn’t guaranteed. About 6% of people end up with permanent nerve damage, even after stopping the drug.
Physical therapy helps. People who do structured rehab-balance training, gentle stretching, sensory retraining-recover 37% faster than those who don’t. Pain meds like gabapentin or pregabalin can ease discomfort, but they don’t fix the nerve. Only time and stopping the drug can do that.
What to Do Next: A Practical Plan
If you’re currently on metronidazole:
- Check how much you’ve taken. Multiply your daily dose by the number of days. If you’re over 42 grams, talk to your doctor about switching.
- Ask your doctor if you really need to keep taking it. Is there a safer alternative? Could a shorter course work?
- Start checking your hands and feet daily. Use a cotton swab to lightly touch your toes and fingertips. If you can’t feel it, that’s a red flag.
- If you have symptoms, stop the drug immediately. Don’t wait for a follow-up appointment.
- Request a referral to a neurologist. Bring your dosage history and symptom timeline.
If you’re a doctor:
- Use the Total Neuropathy Score-a simple questionnaire-to screen patients on extended therapy.
- Set electronic alerts in your EHR to flag metronidazole prescriptions beyond 28 days.
- Ask patients: "Have you noticed any numbness or tingling in your hands or feet?" Don’t assume they’ll volunteer it.
- Consider alternatives like fidaxomicin for C. diff, or clindamycin for anaerobic infections when appropriate.
What’s Changing in 2025
The FDA updated metronidazole labels in 2023 to highlight the 42-gram threshold. Hospitals like Mayo Clinic now block prescriptions beyond 28 days without infectious disease approval. That’s progress.
But the real game-changer might be blood testing. A clinical trial at UCSF is testing whether checking metronidazole levels in the blood can help personalize dosing and prevent toxicity. Early results suggest that patients with higher blood concentrations are at much greater risk-even if their total dose is under 42 grams.
By 2025, experts predict routine serum monitoring will become standard for anyone on metronidazole longer than two weeks. That could cut neuropathy cases by 60-70%.
For now, the best protection is awareness. Know the signs. Track your dose. Speak up if something feels off.
Final Thought: This Isn’t Just a Side Effect-It’s a Warning
Metronidazole is a powerful tool. But like any tool, it can hurt you if you don’t use it carefully. The numbness, the tingling, the burning-they’re not minor inconveniences. They’re your nerves sending an SOS. Ignoring them doesn’t make them go away. It just gives them more time to do permanent damage.
Don’t wait for a diagnosis. If you’re on metronidazole and your feet feel strange, stop. Talk to your doctor. Ask if you’ve crossed the 42-gram line. And if you’re not sure, assume you have.
Can metronidazole cause permanent nerve damage?
Yes, in about 6% of cases, metronidazole-induced neuropathy leads to permanent nerve damage, even after stopping the drug. Most people recover fully, but recovery can take months, and delays in stopping the medication increase the risk of lasting harm. Early discontinuation is the best way to prevent permanent injury.
How long does it take for metronidazole neuropathy to go away?
Symptoms usually start improving within 2-4 weeks after stopping metronidazole, but full recovery can take 3 to 8 months. Some patients need physical therapy to regain strength and sensation. The sooner you stop the drug, the faster and more complete your recovery is likely to be.
Is metronidazole neuropathy common?
It’s underreported, not uncommon. While only about 1-2% of patients on short courses develop neuropathy, the risk jumps to nearly 18% in those who exceed 42 grams total. With over 10 million metronidazole prescriptions in the U.S. each year, thousands are at risk-especially those on long-term therapy for chronic infections.
Can I take metronidazole again if I had neuropathy before?
No. Once you’ve developed metronidazole-induced neuropathy, you should avoid the drug entirely. Re-exposure-even at lower doses-can trigger a rapid return of symptoms, often more severe than before. Your nerves are more vulnerable after the first episode.
What are the alternatives to metronidazole?
Alternatives depend on the infection. For bacterial vaginosis, clindamycin cream or vaginal tablets work well. For C. diff, fidaxomicin is preferred over metronidazole for recurrent cases. For anaerobic infections, penicillin derivatives or carbapenems may be options. Always discuss alternatives with your doctor-don’t assume metronidazole is the only choice.
Does vitamin B12 help with metronidazole neuropathy?
While vitamin B12 deficiency can cause similar nerve symptoms, there’s no strong evidence that taking extra B12 reverses metronidazole damage. However, correcting any existing deficiency is still important for overall nerve health. Some research is testing alpha-lipoic acid as a protective agent, but it’s not yet standard treatment.
Should I get an EMG if I have tingling from metronidazole?
An EMG can confirm nerve damage and rule out other causes like diabetes or spinal issues. But you shouldn’t wait for testing to stop the drug. If your symptoms match metronidazole neuropathy and you’ve taken more than 42 grams, stop the medication immediately. The EMG can follow later to track recovery.
Can metronidazole cause numbness in the face or arms?
Yes. While symptoms usually start in the feet and hands, they can spread upward. Numbness in the arms, fingers, or even the face has been reported in severe cases, especially with very high cumulative doses. The pattern is still symmetric, but it’s not limited to the lower body.
Next Steps: What to Do If You’re at Risk
If you’re on metronidazole and haven’t hit 42 grams yet, ask your doctor: "Is this course necessary? Can we switch to a shorter treatment or a different antibiotic?" Keep a log of your daily dose and total days. Set a calendar reminder to check your symptoms every week.
If you’ve already crossed the threshold and have symptoms, stop the drug now. Don’t wait for your next appointment. Call your doctor and ask for a neurology referral. Bring your dosage history. If you’re in pain, ask about physical therapy options.
Metronidazole saved lives. But it can also steal them-slowly, silently, through numb toes and burning feet. You don’t need to be a doctor to recognize the warning signs. You just need to listen to your body.


13 Responses
Just got off a 6-week course for C. diff and noticed my toes went numb last week. Thought it was my shoes. This post scared the hell out of me but also saved my nerves. Stopped the meds yesterday and booked a neuro appointment. If you’re on this drug longer than a week, check your feet daily. Seriously.
I’ve been on metronidazole for 3 months for a liver abscess and my hands feel like they’re buzzing. I thought it was just stress. I didn’t realize it could be the drug. I’m going to ask my doctor about alternatives tomorrow.
My mom took this for diverticulitis and ended up in physical therapy for 6 months. She still gets tingling in her fingers sometimes. Doctors never warned us. This needs to be standard info.
Big Pharma knows this happens and hides it. They don’t want you stopping the drug because it’s too profitable. The FDA update? A PR stunt. They’ll keep pushing it until someone sues them. Watch the lawsuits start next year.
Wow you people are so dramatic. I’ve taken this like 10 times and never had numbness. Probably just anxious hypochondriacs making it up.
Why is the FDA only updating labels now? In other countries they monitor this like a war crime. We’re falling behind because Big Pharma owns our regulators. If you’re on metronidazole, you’re basically gambling with your nervous system. And we wonder why healthcare is broken.
My sister had this after 8 weeks. She couldn’t walk without holding onto walls. Took her 5 months to get back to normal. I’ve been tracking my dose since reading this. 34 grams so far. I’m stopping at 40. Better safe than sorry.
Thank you for this comprehensive and clinically grounded overview. The emphasis on early recognition and dose tracking is essential. I am a primary care physician and will be implementing the Total Neuropathy Score in my practice immediately. Additionally, I will be setting automated alerts in our EHR system for prescriptions exceeding 28 days. Early intervention saves function. This is public health advocacy at its finest.
As someone who’s lived in three countries, I’ve seen how differently this drug is handled. In India, they use it like candy. In Germany, they test blood levels after 14 days. We need a global standard. Not just warnings-actual monitoring protocols. This isn’t just American medicine failing. It’s systemic.
Just stopped my 5th day of metronidazole after reading this. 🙏 Thank you for sharing. I’m going to ask for fidaxomicin next time. My feet were already tingling a little. Better safe than sorry. 💪
Idk man. I just take what the doc gives me. Too much thinking.
They’re not just hiding this-they’re weaponizing it. The same people who pushed opioids are pushing this. They know people will suffer quietly. They count on your silence. Your numb toes? That’s their profit margin. Wake up. This isn’t medicine. It’s corporate violence.
While I appreciate the intent and the detailed clinical observations presented herein, I must respectfully posit that the assertion regarding the 42-gram threshold, while statistically significant in certain cohort studies, lacks sufficient longitudinal validation across diverse demographic populations. Moreover, the conflation of peripheral neuropathy with autonomic dysfunction, while clinically plausible, may inadvertently induce iatrogenic anxiety in patients who present with non-specific somatic symptoms. The absence of controlled trials demonstrating causality beyond correlation, coupled with the confounding influence of preexisting metabolic conditions such as diabetes mellitus and vitamin B12 deficiency, renders the blanket recommendation to discontinue therapy upon reaching 42 grams potentially premature and, in certain clinical contexts, contraindicated. A more nuanced, individualized risk-benefit analysis, incorporating pharmacokinetic profiling and genetic polymorphisms in drug-metabolizing enzymes, would be preferable to population-based thresholds.