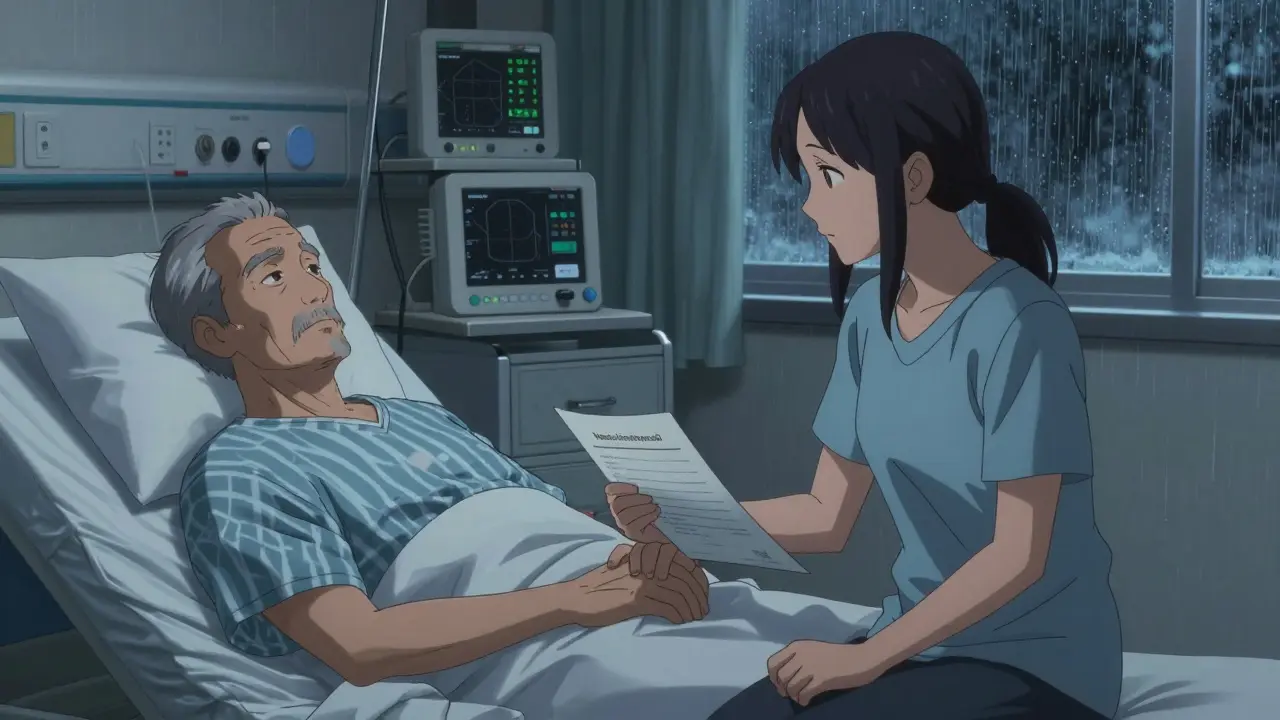
Imagine you’re in the hospital after a stroke. You can’t speak. The doctors ask your family: Do you want him on antibiotics? Should we give him pain meds? What about blood thinners? No one knows your real wishes. That’s not hypothetical. It happens every day. And it’s avoidable.
Most people don’t think about medical decisions until it’s too late. But if you’ve ever watched someone you love struggle in a hospital bed, unsure if they’d want to keep going, you know how painful that uncertainty is. A Medical Power of Attorney isn’t just paperwork. It’s a way to make sure your voice is heard-even when you can’t speak.
What Exactly Is a Medical Power of Attorney?
A Medical Power of Attorney (also called a Healthcare Proxy or Durable Power of Attorney for Health Care) is a legal document that lets you pick someone you trust to make medical decisions for you if you ever lose the ability to speak for yourself. It doesn’t kick in while you’re alert and able to talk. It only activates when doctors determine you can’t make or communicate your own choices.
This isn’t the same as a living will. A living will lists specific treatments you do or don’t want-like no ventilators or no CPR. But life doesn’t always fit neatly into those boxes. What if you develop a new infection? What if a new medication could help but wasn’t around when you signed your living will? That’s where a healthcare proxy shines. Your agent can make decisions based on what they know about your values, not just what’s written on paper.
In every U.S. state, this document is legally recognized. Some states require two witnesses who aren’t family or potential heirs. Others need a notary. A few, like California, only need your signature. But no matter where you live, the core idea is the same: give someone you trust the legal right to act on your behalf.
Why Medication Decisions Are the Most Common Point of Conflict
Studies show that the biggest fights in ICUs aren’t about ventilators or feeding tubes. They’re about medications.
Is it okay to give painkillers if they might make breathing harder? Should antibiotics be used if they’re not guaranteed to work? Do we keep giving blood thinners if the risk of bleeding is rising? These aren’t yes-or-no questions. They’re messy, emotional, and deeply personal.
A 2023 study in the Journal of Pain and Symptom Management found that patients with a designated healthcare proxy had 32% fewer medication-related conflicts during hospital stays. Why? Because their agent knew their priorities. Maybe you’d rather be comfortable than live longer. Maybe you’d fight for every chance. Your agent needs to know which side of that line you’re on.
But here’s the catch: many agents don’t know. A 2022 survey by The Conversation Project found that 41% of agents felt uncertain about medication preferences-even after signing the paperwork. One woman in Indiana refused blood thinners because she thought her father hated all meds. He’d actually said he wanted them if they could prevent a stroke. He had one anyway. It was preventable.
How to Talk About Medication Preferences (Without Making It Weird)
You don’t need a medical degree to have this conversation. You just need honesty.
Start simple. Ask yourself: What matters most to me if I’m sick? Is it comfort? Being at home? Avoiding pain? Staying alert? Then talk to your agent.
Use real examples:
- “If I have an infection and I’m confused, I want antibiotics-even if I’m not sure I want them. I don’t want to die from something treatable.”
- “I’m okay with strong pain meds, even if they make me sleepy. I’d rather be calm than in pain.”
- “I don’t want to be on meds that just prolong the dying process. If my body is shutting down, I want to be held, not hooked up.”
Don’t just say “I don’t want to be a burden.” Say what that looks like in real terms. Do you mean no IVs? No feeding tubes? No daily pills? Be specific.
Write it down. Not just on the form. On a note in your phone. In a letter to your agent. Include names of medications you’ve had bad reactions to. Mention if you’ve ever refused a drug because it made you feel like a different person.
The more details you give, the less your agent has to guess.
What Your Agent Can and Can’t Do
Your agent doesn’t have unlimited power. They can’t override state laws. They can’t demand treatments doctors say are useless or harmful. They can’t ignore your documented wishes.
But they can:
- Decide whether to give you oral meds or injections
- Ask for second opinions
- Request pain management
- Refuse treatments you’ve said you don’t want
- Access your medical records
- Decide if you go to the hospital or stay home
Some states limit what agents can do with psychiatric meds. Indiana, for example, requires a doctor to sign off before a proxy can refuse antipsychotics. Always check your state’s rules. Most state health departments offer free forms online. LawHelp DC and the Indiana Health Care Quality Resource Center are good places to start.
And remember: your agent can’t act on your behalf until two doctors confirm you’re unable to make decisions. That’s not a loophole. It’s a safeguard.
Why a Living Will Isn’t Enough
A living will is like a GPS that only knows your destination. A Medical Power of Attorney is like having a friend in the car who knows your driving style, your tolerance for traffic, and whether you’d rather take the scenic route even if it’s slower.
Most living wills only cover end-of-life scenarios. What if you get pneumonia? What if you have a bad reaction to a new drug? What if you’re in a coma but not dying? Living wills don’t cover those. But your agent can. They can read the situation, talk to doctors, and make a call based on what they know about you-not just what’s written in 2018.
That’s why experts say you need both. A living will for clear-cut situations. A healthcare proxy for everything else.
POLST and Other Tools: What Else Should You Know?
If you have a serious illness-like advanced cancer, heart failure, or late-stage dementia-you might also want a POLST form (Physician Orders for Life-Sustaining Treatment). This isn’t a substitute for a Medical Power of Attorney. It’s a supplement.
POLST is a medical order, signed by a doctor, that tells EMS and hospitals exactly what to do. It covers things like:
- Do not resuscitate (DNR)
- Do not intubate
- Use antibiotics
- Use feeding tubes
- Use IV fluids
It’s designed for people who are likely to die within a year. It’s honored in 47 states. And by December 2025, all Medicare/Medicaid facilities must have electronic POLST systems in place. If you’re in that group, talk to your doctor about combining POLST with your Medical Power of Attorney.
Common Mistakes (And How to Avoid Them)
People mess this up in predictable ways.
Mistake 1: Picking someone because they’re the oldest kid, not because they’re the most thoughtful.
Don’t default to the eldest child. Pick the person who listens, who remembers your jokes, who knows you’d rather die at home than in a hospital. Someone who won’t be swayed by guilt or pressure from other family members.
Mistake 2: Signing the form and never talking about it.
Over a third of agents in a University of Pennsylvania study said they wished the person had told them more about pain meds. Don’t be that person. Have the conversation. Twice. Once when you’re healthy. Once when you’re sick.
Mistake 3: Assuming the hospital will find your paperwork.
Most hospitals don’t automatically check for advance directives unless you tell them. Keep a copy in your wallet. Email it to your agent. Put it in your phone’s health app. Tell your primary doctor to add it to your chart.
Mistake 4: Thinking it’s done after one signing.
Update it every year. Or after any big change: divorce, new diagnosis, a move, or if your agent moves away. Life changes. Your wishes might too.
What Happens If You Don’t Have One?
If you don’t name an agent, the law steps in. Usually, it’s your spouse, then adult children, then parents. But what if you’re unmarried? What if your kids fight? What if your mom hates hospitals but your dad wants everything done?
That’s when courts get involved. That’s when delays happen. That’s when you get treatments you’d never have wanted-because no one knew better.
And it’s not just about you. It’s about them. The people who love you. They shouldn’t have to guess what you’d want. They shouldn’t carry guilt because they chose wrong.
Where to Start Today
You don’t need a lawyer. You don’t need to pay anything.
Go to your state’s health department website. Search for “medical power of attorney form [your state].” Download it. Print it. Sit down with your agent. Have coffee. Talk about meds. Talk about pain. Talk about dignity.
Then sign it. Two witnesses. Or a notary. Done.
And then? Tell your doctor. Email it to your agent. Put it in your phone. Make sure everyone who might be in the room when it matters knows where to find it.
This isn’t about death. It’s about control. About respect. About making sure the last decisions made about your body are the ones you’d have made-if you could.
Do it now. Not tomorrow. Not when you’re older. Now.
Can my agent override my living will?
No. Your agent must follow your written wishes in your living will. If your living will says no ventilators, your agent can’t demand one. But if your living will doesn’t cover a new situation-like a sudden infection-your agent can make a decision based on what they know about your values.
Do I need a lawyer to create a Medical Power of Attorney?
No. Most states offer free, state-approved forms online. You just need to sign it in front of two witnesses (who aren’t family or heirs) or a notary. A lawyer is only necessary if your situation is complex-like owning a business, having multiple families, or dealing with psychiatric conditions.
Can my agent make decisions about psychiatric medications?
It depends on your state. In Indiana, for example, a doctor must sign off before your agent can refuse antipsychotics. In other states, agents have full authority. Always check your state’s rules. If you have a mental health condition, it’s even more important to discuss your wishes clearly with your agent and doctor.
What if my family disagrees with my agent?
Your agent has legal authority. Hospitals must follow their decisions if the document is valid. But family fights still happen. That’s why clear communication is key. Talk to your family about your choice. Explain why you picked your agent. Write it down. The more you’ve documented your wishes, the harder it is for others to challenge them.
How often should I update my Medical Power of Attorney?
At least once a year. And definitely after major life changes: divorce, new diagnosis, moving to a new state, or if your agent becomes unable to serve. Your values might change too. What you wanted at 50 might be different at 70. Revisit your choices regularly.
Can I name more than one agent?
You can name a primary agent and a backup. But naming two people to act together often causes delays and conflict. If they disagree, decisions stall. It’s better to pick one person you trust completely, and name a clear backup if they can’t serve.

13 Responses
My dad refused blood thinners because he thought they were 'poison.' He had a stroke two weeks later. We never talked about it. Don't be us.
Stop gaslighting people into thinking this is about 'control.' It's about fear. You're just scared of dying so you buy legal paperwork like it's a security blanket. Real people don't think this way.
This hit me right in the chest 💔
My mom had a stroke and we had NO idea what she'd want. The guilt? Unbearable. I'm printing this out and having the talk with my sister tonight. Thank you for saying this.
There's a fundamental epistemological flaw in assuming that a proxy can 'represent' your values. Values are emergent, not static. You can't encode ontological preferences into a legal document. The proxy becomes a performative artifact of neoliberal autonomy theater.
Just did this with my wife last weekend. We sat on the porch with iced tea and talked about pain meds, antibiotics, and whether we'd want to be 'kept alive' if we couldn't recognize each other. Didn't feel morbid. Felt like love.
Do it. Now. Not later.
Bro, in India we don't even have access to these forms half the time. My cousin's mom died in a rural hospital because they didn't know what 'DNR' meant. This is a privilege conversation. But if you can do it? Do it. And help someone who can't.
Oh wow, another sanctimonious lecture from the 'I've-read-a-medical-blog-so-now-I-know-better' crowd. You think your little form will save anyone? Hospitals ignore these all the time. Your 'agent' is just another person who'll break down crying and say 'do everything' when the time comes. This is performative self-help garbage.
my wife is my agent and i told her i dont want to be on no machines but i never said anything about meds… now im scared shes gonna guess wrong. i need to talk to her again before i forget. thanks for the kick in the pants
There is a quiet dignity in surrendering control. But perhaps the real act of autonomy is not in writing a document, but in naming the fear behind it. The proxy is not a shield-it is an invitation to be known.
As a healthcare administrator I have seen too many families fight over this. The form is meaningless without communication. Document your wishes. Then have the conversation. Then document the conversation. Repeat annually. This is not optional. It is responsibility.
There is a grammatical error in the article. The phrase 'two witnesses who aren't family or potential heirs' should be 'two witnesses who are not family members or potential heirs.' Precision matters in legal documents. This is not semantics. It is law.
My grandfather died in a hospital in Punjab. They gave him IVs he never wanted because no one knew. We cried for years. Now I’ve told my daughter: ‘If I’m not laughing, don’t keep me alive.’ I wrote it on my phone. I told my doctor. I gave my sister a copy. No more guessing. No more guilt.
Do it. For them. Not for you.
It's fascinating how this entire discourse is framed as an individualistic act of agency, when in reality, the structural failures of the healthcare system-underfunded palliative care, lack of cultural competency, insurance-driven triage-are what force people into this performative legal choreography. The proxy is a Band-Aid on a hemorrhage.