HIV Protease Inhibitor Comparison Tool
Select Two PIs to Compare
Key Features Overview
Click "Compare" to see detailed information about selected drugs.
Drug Characteristics
Select two drugs to compare their features.
Clinical Recommendations
Based on your selections, consider these points:
- Indinavir requires strict hydration to prevent kidney stones.
- Darunavir has the highest resistance barrier among PIs.
- Atazanavir and Darunavir offer once-daily dosing.
- Consider lipid profiles when choosing between agents.
Quick Takeaways
- Indinavir offers strong viral suppression but demands strict hydration and dosing schedules.
- Saquinavir and ritonavir are older, cheaper options but have more drug‑drug interactions.
- Atazanavir and darunavir provide once‑daily dosing and better tolerability for many patients.
- Resistance patterns differ: darunavir retains activity against most protease‑inhibitor‑resistant strains.
- Cost and insurance coverage vary widely; newer agents may be pricier but often have lower overall healthcare costs due to fewer side‑effects.
What Is Indinavir?
When building an HIV treatment plan, Indinavir is a protease inhibitor (PI) that blocks the HIV‑1 protease enzyme, preventing viral particles from maturing into infectious forms. Approved in 1997, it is supplied as Indinavir Sulphate tablets, typically taken at a dose of 800mg three times daily.
Key attributes of indinavir include:
- Peak plasma concentration: reached within 1-2hours.
- Half‑life: about 1.5hours, which drives the need for multiple daily doses.
- Hydration requirement: patients should drink at least 1.5L of water per day to avoid kidney stones.
How Indinavir Stacks Up Against Other Protease Inhibitors
To decide whether indinavir is right for a particular person, compare it across four practical dimensions: efficacy, resistance barrier, side‑effect profile, and convenience.
Efficacy
Clinical trials from the late‑1990s showed indinavir reduces viral load by an average of 1.5-2 log10 copies/mL when combined with two nucleos(t)ide reverse transcriptase inhibitors (NRTIs). Newer agents such as darunavir achieve similar or slightly better reductions, often in the 2‑log range, with faster time‑to‑suppression because of higher potency.
Resistance Barrier
If the virus mutates, indinavir loses potency after just a few key mutations (e.g., V82A, I84V). In contrast, Darunavir holds the highest genetic barrier among PIs, remaining active against many resistant strains.
Side‑Effect Profile
| Drug | Kidney stones | Metabolic changes | GI intolerance | Drug‑drug interactions |
|---|---|---|---|---|
| Indinavir | High (≈5-7%); hydration critical | Moderate (↑ cholesterol, triglycerides) | Occasional nausea | Moderate; CYP3A4 substrate |
| Saquinavir | Low | High (significant lipid elevations) | Frequent dyspepsia | High; boosters needed |
| Ritonavir | Low | Very high (hyperglycemia, lipodystrophy) | Common nausea, diarrhea | Very high; strong CYP3A4 inhibitor |
| Lopinavir/ritonavir | Low | High (cholesterol, triglycerides) | Moderate GI upset | High; requires ritonavir booster |
| Atazanavir | Low | Low (minimal lipid impact) | Occasional jaundice (hyperbilirubinemia) | Moderate; boosted with ritonavir if needed |
| Darunavir | Low | Low to moderate | Rare GI issues | Moderate; boosted for full effect |
Convenience and Dosing
Indinavir’s short half‑life means patients take it three times a day, often with food and a glass of water. Saquinavir also needs multiple daily doses unless boosted. Lopinavir/ritonavir is taken twice daily, but the syrup formulation can be cumbersome.
Atazanavir and darunavir are the most convenient: both can be taken once daily when boosted, reducing pill burden and improving adherence.
Cost Considerations (2025 market)
Generic indinavir has dropped to aboutAU$15 per tablet, making a monthly supply roughlyAU$1,200. Saquinavir generic is slightly cheaper, while ritonavir remains low‑cost because it’s often used as a booster.
Atazanavir and darunavir, though still under patent in some regions, are priced higher (≈AU$35-45 per tablet). However, insurance plans frequently cover them because of their better tolerability and lower downstream healthcare expenses.
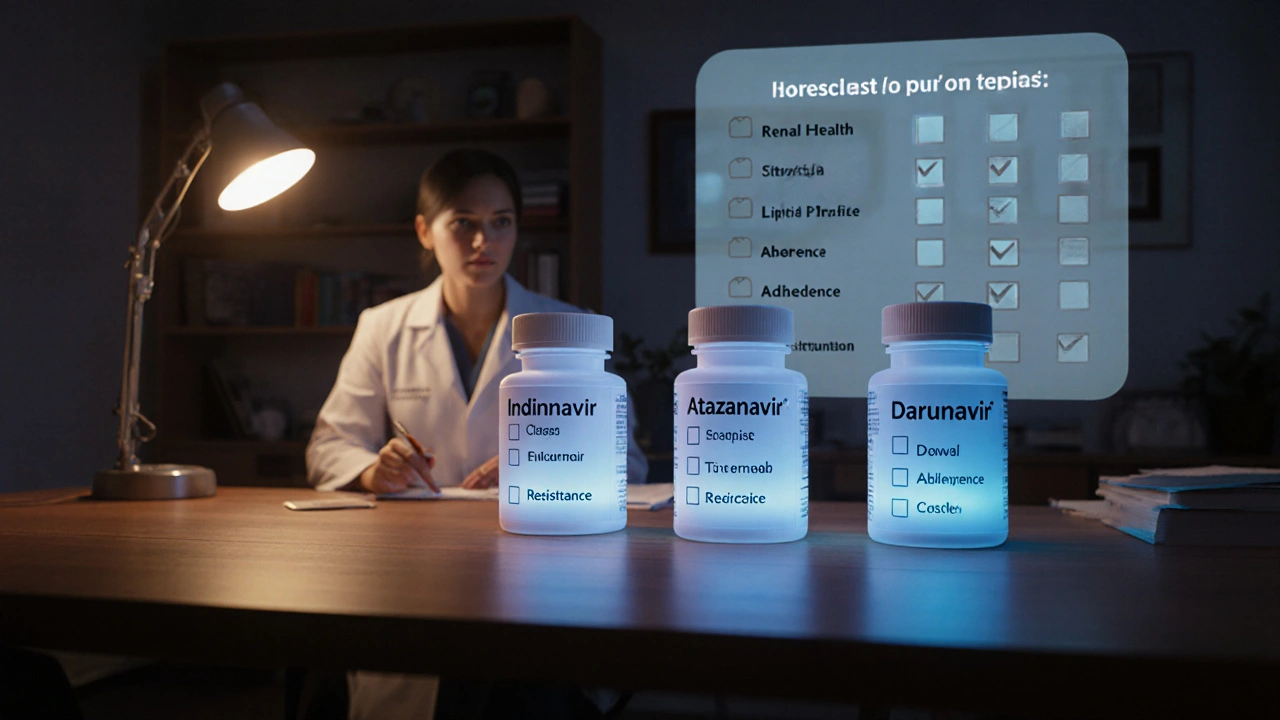
Choosing the Right Protease Inhibitor
Use the following checklist to match a patient’s clinical picture with the most suitable PI.
- Renal health: If the patient has a history of kidney stones or reduced GFR, steer clear of indinavir.
- Lipid profile: For hyperlipidemic patients, avoid saquinavir or lopinavir/ritonavir; favor atazanavir or darunavir.
- Adherence potential: Once‑daily regimens (atazanavir, darunavir) are best for patients with busy schedules.
- Resistance history: If prior PI failure occurred, choose darunavir for its high barrier.
- Drug‑interaction load: Patients on multiple CYP3A4 substrates should avoid ritonavir‑boosted combos.
- Cost constraints: When budget is tight and renal function is normal, indinavir remains a viable low‑cost option.
Practical Tips When Prescribing Indinavir
- Instruct patients to drink at least 1.5L of water daily and to empty the bladder frequently.
- Schedule dosing with meals to improve absorption and reduce GI upset.
- Monitor serum creatinine and urinalysis every 3-6months for early signs of nephrolithiasis.
- Check lipid panel at baseline and after 12weeks; consider statin therapy if needed.
- Review all concomitant meds for CYP3A4 interactions; avoid co‑administration with warfarin or certain anti‑epileptics.
Frequently Asked Questions
Is indinavir still recommended in first‑line HIV therapy?
Guidelines now favor integrase‑strand transfer inhibitors for most treatment‑naïve patients, but indinavir remains an option when cost is a major factor and the patient has no renal risk.
Can indinavir be taken with food?
Yes. Taking indinavir with a moderate‑fat meal improves bioavailability, but avoid high‑fat meals that can delay absorption and increase side‑effects.
What are the signs of indinavir‑related kidney stones?
Patients may report flank pain, hematuria, or sudden difficulty urinating. Prompt imaging and increased hydration usually resolve the issue.
How does darunavir’s resistance profile compare?
Darunavir retains >95% activity against viruses that have accumulated up to three major PI mutations, making it the go‑to choice after PI failure.
Are there any food restrictions with atazanavir?
Atazanavir should be taken with a meal containing at least 250kcal of fat; otherwise, absorption drops significantly.
Bottom Line
If you need a low‑cost, well‑studied PI and can manage the hydration requirement, indinavir still has a place in therapy. However, for most patients today, newer agents like atazanavir or darunavir offer smoother daily routines, fewer metabolic side‑effects, and stronger resistance barriers, even if they carry a higher price tag. The best choice always aligns with the individual’s kidney function, lipid status, adherence capacity, and insurance coverage.


10 Responses
Indinavir remains a viable low‑cost option as long as patients commit to the required hydration regimen.
I understand the concern about kidney stones and appreciate how a simple water intake habit can make a big difference.
When we look at indinavir, we see more than a pill; we see a mirror reflecting the trade‑offs of modern medicine.
It forces us to ask why we accept a drug that demands three daily doses.
Is convenience more important than the discipline it teaches?
The hydration rule feels like a ritual, a daily reminder that our bodies demand respect.
Some people call it burdensome, others call it empowering.
In the end, the choice is personal, yet it is shaped by the healthcare system that prices drugs by the tablet.
Cost‑savings can feel like a victory when a generic is cheap, but hidden costs like stone formation can offset that win.
Doctors who prescribe indinavir often do so because they understand a patient’s lifestyle and can monitor kidney health.
If you think about the chemistry, indinavir’s short half‑life is what makes it potent but also demanding.
It is a reminder that the virus can be clever, and our therapy must be even cleverer.
Every dose taken with a glass of water becomes a tiny act of rebellion against viral replication.
Some patients love that rhythm, others dread it, but both experiences teach us about adherence.
Education on hydration can turn a side‑effect into a health habit that improves overall wellness.
And when the water bottle empties, it’s a cue to check labs, to stay engaged with care.
So, whether you love or loathe indinavir, recognize that its story is woven into the broader narrative of HIV treatment 😊.
For clinicians, the key takeaway is to assess renal function before starting indinavir, ensure the patient can meet the 1.5 L daily water intake, and schedule regular creatinine checks; this mitigates most stone‑related complications.
Older protease inhibitors like indinavir and saquinavir are relics that belong in a museum, not in modern regimens; their side‑effect profiles are unacceptable when safer, once‑daily options exist.
Hey, just wanted to add that even if indinavir seems old, it's still a good choice for many, especially when insuranc covers it 🧡.
From a cultural standpoint, the availability of a cheap generic like indinavir can make a huge difference in low‑resource settings where newer drugs are out of reach.
Of course, the pharma giants probably want us to believe that newer PIs are the only safe path, while they keep the old stuff cheap to keep the market fragmented and confusing – classic corporate misdirection.
Let’s stay positive – regardless of the marketing games, patients and providers can make informed choices that balance cost, convenience, and safety, leading to better outcomes for everyone.
Interesting how the “cutting‑edge” label gets slapped on any new pill, yet the fundamentals of adherence and side‑effect management remain unchanged – classic hype.