When you pull an old bottle of pills from the back of your medicine cabinet, you might think, "It’s just a few months past the date-should I still take it?" But here’s the truth: expired drugs don’t just lose strength. They can change in ways you can see, smell, or feel-and those changes aren’t always harmless.
What Happens to Medicines After They Expire?
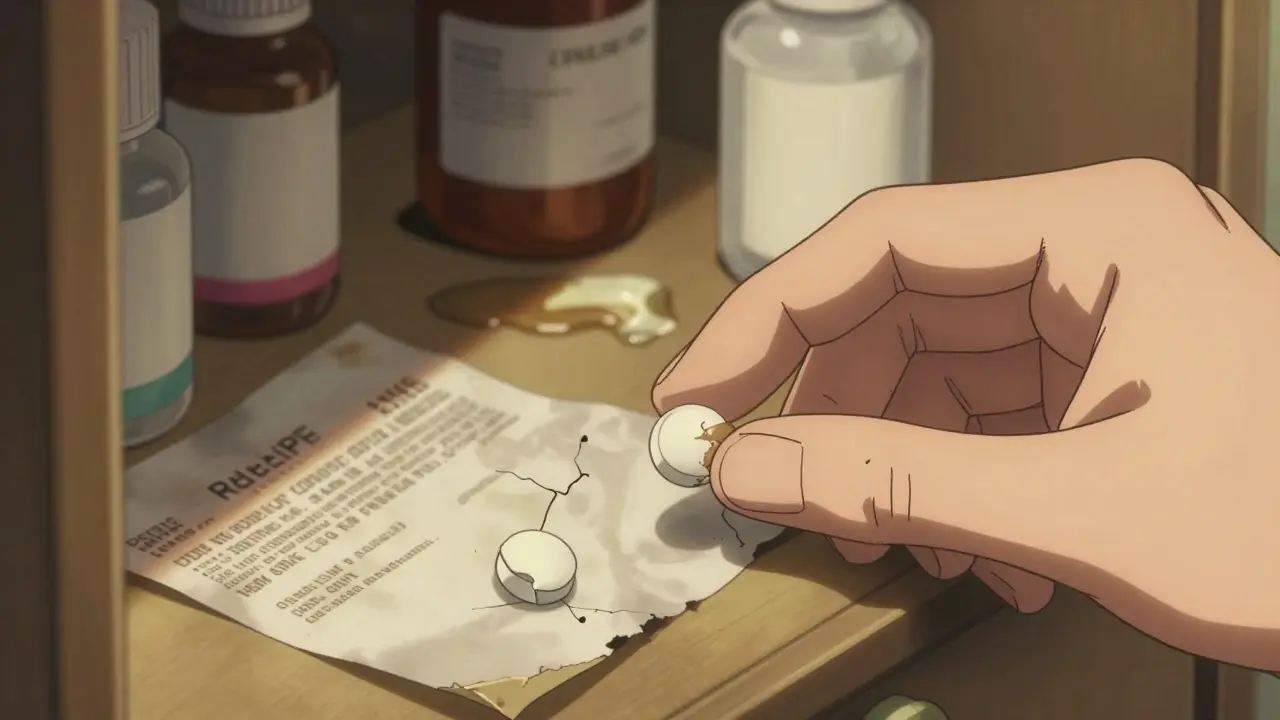
Every drug has an expiration date for a reason. That’s not just a marketing tactic or a legal formality. It’s based on real science. Manufacturers test medicines under controlled heat, humidity, and light to see how long they stay stable. Once that date passes, the chemical structure can break down. That’s when color, odor, and texture start to shift.Take tetracycline, for example. When it degrades, it turns from white to yellow or brown. That’s not just cosmetic. Degraded tetracycline can damage your kidneys. Or consider nitroglycerin, used for heart attacks. If it turns from clear to yellow-brown, it’s lost potency. In an emergency, that could be deadly.
It’s not just about pills. Creams, liquids, and injections all change too. A tube of hydrocortisone cream that separates into oily and watery layers? That’s not normal. A liquid antibiotic with tiny floating particles? That’s a red flag. These aren’t just "looks bad" issues-they’re safety signals.
How to Check for Color Changes
Color change is the most common sign of degradation. According to NASA’s 2011 stability study, 68.3% of expired medications showed visible discoloration. Solid tablets? Look for spots, streaks, or uneven coloring. A white pill with brown edges? That’s not aging gracefully-it’s breaking down.For liquids, check for cloudiness or unusual tinting. Clear eye drops that look cloudy? Throw them out. Yellowing of a once-clear solution? That’s a sign of oxidation. Even subtle shifts matter. A pill that was bright white and now looks dull gray? Don’t risk it.
Here’s a simple trick: compare it to a fresh bottle if you have one. If you don’t, look up reference images from the FDA’s Drug Expiration Database. Some pharmacies keep sample images of how their medications should look. If you’re unsure, don’t guess. Call your pharmacist.
Smell: The Forgotten Warning Sign
Most people don’t think to smell their medicine. But odor changes are a powerful clue. A bottle of amoxicillin capsules that smells musty or sour? That’s not the usual pill odor. That’s moisture getting in, causing the active ingredient to break down.Some drugs, like aspirin, naturally smell faintly of vinegar when they degrade. That’s acetic acid forming as the compound breaks apart. It’s not just unpleasant-it means the drug is losing its effectiveness. If your pain reliever smells like old vinegar, don’t take it.
For creams and ointments, a rancid or chemical smell often means the oil base has gone bad. That can irritate skin or even cause infection if applied to broken skin. If it smells "off," even slightly, treat it as expired.
Texture: Feel the Difference
Texture changes are easy to miss-but they’re just as important. Take a tablet. If it crumbles when you handle it, that’s friability. It’s lost its structural integrity. That means the drug may not dissolve properly in your stomach, so you’re not getting the right dose.Capsules? If the powder inside is clumped together or feels sticky, moisture has gotten in. That’s especially common with hygroscopic drugs like amoxicillin. Once moisture enters, chemical reactions accelerate. The drug can become less effective-or even toxic.
Creams and gels should be smooth and uniform. If you see oil floating on top or water pooling at the bottom, that’s phase separation. It means the emulsion has broken. That’s not just messy-it’s unsafe. The active ingredient is no longer evenly distributed. You might apply a dose that’s too strong in one spot and too weak in another.
Liquids? Look for sediment or floating particles. Even tiny specks matter. The U.S. Pharmacopeia says non-sterile liquids should have no more than 6,000 particles larger than 10 micrometers per container. You won’t see that with your eyes, but if you see any visible specks, it’s time to discard it.

Why Visual Checks Alone Aren’t Enough
You might think, "If it looks fine, it’s probably okay." But here’s the catch: physical changes don’t always match chemical degradation. A study from the National Institute of Justice found human visual inspection is only 65.2% accurate at spotting unsafe drugs. That means nearly one in three degraded medications slip through.Some drugs, like PMZ (a painkiller), can lose potency long before they change color or texture. Others, like certain antibiotics, might look perfect but have broken down into harmful byproducts.
That’s why experts recommend using visual checks as a first step-not the final answer. If something looks wrong, don’t take it. But if it looks normal and you’re still unsure, don’t assume it’s safe. Ask a pharmacist. They have access to stability data and can help you decide.
Real-World Mistakes People Make
In 2019, a hospital kept using expired morphine sulfate because it had fine crystals-and staff thought that was normal. Turns out, those crystals meant the drug had degraded. Fourteen patients had adverse reactions.Another case: a patient kept using expired hydrocortisone cream that had separated. They didn’t realize the liquid part was now too thin to deliver the right dose. Their skin rash got worse.
And on Reddit, a pharmacy tech shared how they threw out a bottle of expired ciprofloxacin ointment that had turned to liquid. That’s exactly what NASA’s research predicted: some semisolid drugs liquefy past expiration, even under normal storage.
These aren’t rare. They’re warnings. Most people don’t know what to look for. That’s why so many expired drugs stay in homes-until someone gets sick.
How to Set Up a Simple Safety System
You don’t need fancy tools to keep your medicine safe. Here’s what to do:- Check all medications every 3 months. Don’t wait for expiration dates to pass.
- Keep medicines in a cool, dry place. Heat and humidity speed up degradation. Avoid bathrooms and windowsills.
- Use a white background and good lighting when inspecting. Natural daylight works best.
- Take photos of pills or creams if you notice anything odd. Show them to your pharmacist later.
- Write the discard date on the bottle when you open it. Most liquids lose potency within 28 days after opening, even if the bottle says otherwise.
For families with kids, keep meds out of reach and check them monthly. Kids sometimes sneak pills, and expired ones can be dangerous.

What to Do When You Find a Problem
If you spot a color, odor, or texture change, don’t flush it or toss it in the trash. Many communities have drug take-back programs. Pharmacies like CVS and Walgreens offer free disposal bins. If none are nearby, mix the medicine with coffee grounds or cat litter, seal it in a bag, and throw it in the trash. Never flush unless the label says to.And never use it. Even if it’s "just a little expired." The risk isn’t worth it. A slightly weaker antibiotic might not kill the infection. A degraded heart medication might fail when you need it most.
What’s Changing in the Industry
The field is moving fast. Hospitals now use automated color sensors to detect degradation. Pfizer’s AI system can predict expiration by analyzing microscopic texture changes with 94.3% accuracy. Portable Raman spectrometers-devices that scan drugs with light-are becoming cheaper and more common.But for now, the simplest tool is still the best: your eyes, nose, and fingers. You don’t need a lab to spot a pill that’s turned brown or a cream that’s separated. You just need to know what to look for.
The FDA and WHO both agree: visual inspection remains the most accessible way to catch dangerous changes in low-resource settings. That means if you’re in a small town, on a budget, or just don’t have access to a pharmacy, your senses are your first line of defense.
Don’t wait for someone to tell you it’s unsafe. If it looks, smells, or feels wrong-discard it. Your body will thank you.
Can I still take medicine after the expiration date if it looks fine?
No. Even if a medicine looks normal, it may have lost potency or degraded into harmful substances. Some drugs, like insulin or nitroglycerin, become ineffective without visible changes. Always assume expiration dates mean "do not use after."
What’s the most common sign that a drug has expired?
Discoloration is the most common sign. Studies show over 68% of expired medications show visible color changes-like white pills turning yellow or clear liquids becoming cloudy. Tablets with brown spots or creams that darken are strong indicators of degradation.
Do all expired drugs become dangerous?
Not all become dangerous, but some can. Antibiotics may not kill infections, leading to worse illness. Heart or seizure meds could fail in emergencies. Degraded tetracycline can harm kidneys. The risk isn’t always obvious, so it’s not worth guessing.
Can I tell if a liquid medicine is bad just by shaking it?
Shaking can help. If a liquid separates into layers and doesn’t remix after shaking, it’s degraded. Suspensions that form clumps or floating particles are unsafe. If you see any visible particles, discard it-even if it’s within the expiration date.
How should I dispose of expired or degraded drugs?
Use a drug take-back program if available. Pharmacies like CVS and Walgreens offer free disposal bins. If none exist, mix the medicine with coffee grounds or cat litter, seal it in a plastic bag, and throw it in the trash. Never flush unless the label specifically says to.
Is it safe to use expired eye drops or ointments?
No. Eye products are especially risky. Even small changes in texture or clarity can introduce bacteria or cause irritation. Expired eye drops can lead to serious infections. Always discard them after the expiration date-even if they look fine.
Can I trust the expiration date on over-the-counter meds?
Yes, but don’t assume it’s safe after that date. Expiration dates are based on strict testing. Once passed, potency drops and degradation begins. For critical meds like epinephrine or heart drugs, never use past the date. For pain relievers, the risk is lower-but still not zero.
Final Thoughts
You don’t need a chemistry degree to protect yourself from expired drugs. You just need to pay attention. Look at the color. Smell the cap. Feel the texture. If anything seems off, don’t take it. Your health isn’t worth the gamble.Keep your medicine cabinet clean, check it every few months, and dispose of anything suspicious. It’s simple. It’s safe. And it could save your life-or someone else’s.

11 Responses
Man, I never thought about how aspirin smells like vinegar when it goes bad-that’s wild. I’ve got a bottle in my bathroom cabinet that’s been there since 2020 and I swear it’s always had that faint tang. Now I’m kinda scared to even open it. Guess I’m cleaning out my medicine cabinet this weekend.
It’s frankly irresponsible how many people treat pharmaceuticals like expired yogurt. The FDA doesn’t set expiration dates because they’re bored-there’s actual pharmacokinetic degradation data behind every single one. And yet, here we are, people popping tetracycline from ‘08 because ‘it still looks white.’ You’re not being resourceful-you’re playing Russian roulette with your renal function.
And don’t even get me started on the ‘I’ll just double the dose’ crowd. Degraded drugs don’t just lose potency-they produce toxic metabolites. You’re not ‘being smart,’ you’re just a walking CDC case study waiting to happen.
Oh sweet mother of mercy, Lori. You sound like you just read the WHO’s 2023 pharmaceutical stability report and decided to become a pharmacist overnight. Chill. Not everyone has access to a pharmacist who’ll answer their 3 a.m. text about a pill’s color. Sometimes, we’re just trying not to die of a sinus infection while living paycheck to paycheck.
Yes, degradation is real. But your tone? It’s the reason people stop asking questions. Maybe try ‘here’s how to stay safe’ instead of ‘you’re a menace to society.’ Just a thought.
68.3% discoloration? That’s not science-that’s a marketing statistic cooked up by someone who sells pill organizers. Also, NASA? NASA studies pharmaceuticals now? Since when did they stop doing space stuff and start analyzing pill stains? I’m calling BS on this entire article.
Stop. Just stop. If it looks weird, don’t take it. If it smells weird, don’t take it. If it feels weird, don’t take it. That’s it. You don’t need a 2000-word essay. You need common sense. Also, ‘phase separation’? Say ‘it’s chunky’.
Interesting piece-though I’d caution against relying solely on visual cues. As the U.S. Pharmacopeia notes, particle counts above 6,000 per container are concerning-but most laypeople can’t discern sub-10-micron particulates. That said, visible sediment, discoloration, or odor shifts are valid red flags. I’ve seen a lot of expired ointments in my time… and yes, the oily separation is a dead giveaway.
Also: thank you for mentioning disposal protocols. So many people still flush meds. Please, please, please don’t do that.
Thank you for this. In Nigeria, we often use expired meds because we can’t afford new ones. But I never knew how to tell if they were dangerous-only if they didn’t work. Now I check the smell, the texture. I’ll show this to my neighbors. 🙏
While the article contains several empirically valid points, its rhetorical approach is alarmist and lacks appropriate nuance. The claim that degraded tetracycline ‘can damage your kidneys’ is technically correct, but the causal chain is overstated without citing LD50 thresholds or clinical incidence rates. Moreover, the reference to NASA’s 2011 stability study is misleading-NASA does not conduct pharmaceutical stability testing. That was conducted by the FDA’s Office of Pharmaceutical Science. Such inaccuracies undermine the credibility of otherwise useful information.
EVERYTHING IS A GOVERNMENT TRAP. 💀 They make the expiration dates short so you keep buying pills. I’ve taken amoxicillin from 2012 and it worked better than the new stuff. Big Pharma doesn’t want you to know this. Also, the FDA is owned by Pfizer. 🚨
Guys, I just checked my cabinet and found a bottle of hydrocortisone that had separated into two layers-I thought it was just old, but now I’m gonna take it to the pharmacy tomorrow. This post literally saved me from a bad rash. Thank you so much for writing this. You guys are awesome. 💪❤️
Actually, I’ve been using a Raman spectrometer app on my phone to scan my meds. It’s not 94.3% accurate like Pfizer’s system, but it’s way better than eyeballing it. You can download it for $19.99 on the App Store. Just point it at the pill and it tells you if the chemical signature matches the original. I’ve been doing this for a year now. Highly recommend.