What Your Prescription Label Really Means
Look at your prescription label. It says "Take 1 tablet twice daily". Sounds simple, right? But how many people actually know what that means in real life? Do you take it at 8 a.m. and 8 p.m.? Or just whenever you remember? If you're unsure, you're not alone. Nearly half of all patients misinterpret basic dosage instructions, and that confusion leads to serious mistakes - missed doses, double dosing, or even dangerous side effects.
The FDA says 43.7% of medication errors tied to prescription labels come from unclear timing. That’s not a small number. It’s one in every two errors. And it’s not because patients aren’t trying. It’s because the language on the label is often vague, outdated, or confusing.
Why "Twice Daily" Is Not Enough
"Twice daily" - or "b.i.d." - is still used on most prescriptions. But here’s the problem: it doesn’t tell you when to take it. For some medications, timing matters just as much as the dose. Blood pressure pills, for example, work best when taken at the same time each day. Antibiotics need to stay at steady levels in your blood - missing a window by a few hours can let bacteria survive and grow stronger.
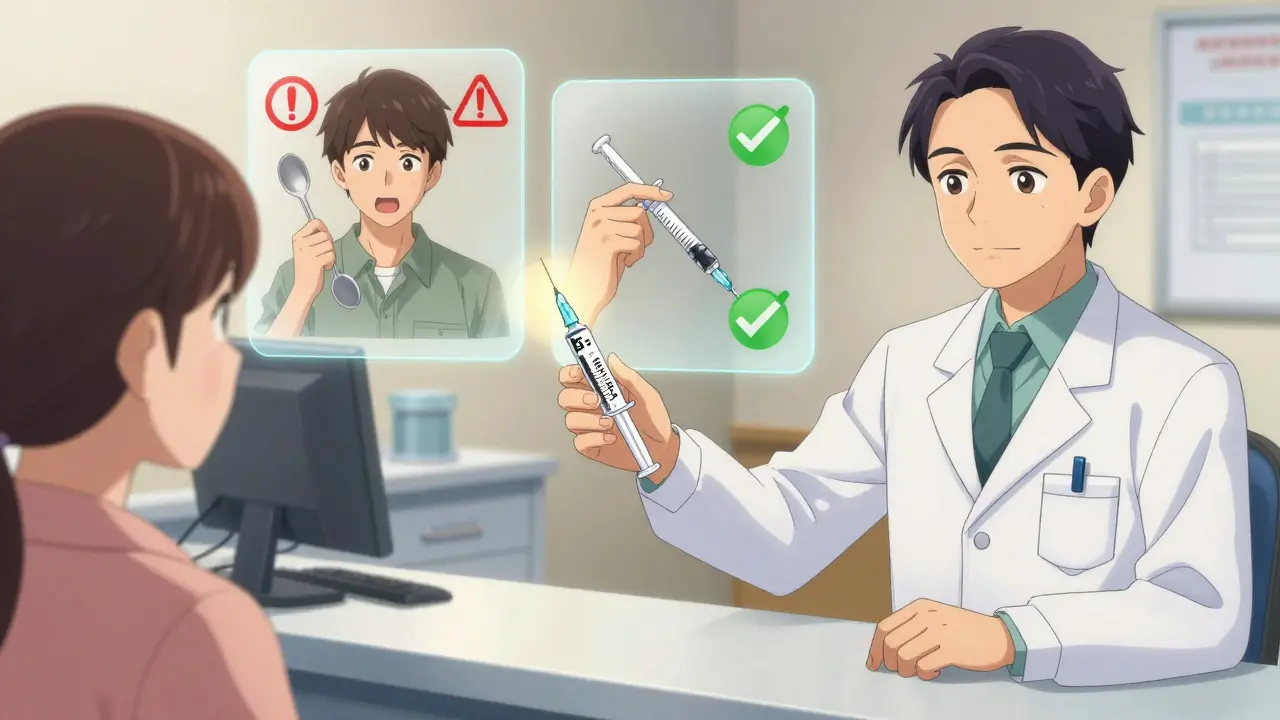
The FDA pushed for clearer language back in 2014. They want labels to say: "Take 1 tablet in the morning and 1 tablet in the evening." That’s specific. It tells you when. It removes guesswork. And studies show it works. At Massachusetts General Hospital, patients who got this clear wording were 34.7% more likely to take their meds correctly.
But most pharmacies still use the old terms. A 2023 study found that 82.7% of retail pharmacy labels still say "twice daily" instead of explicit times. CVS Health changed their system in 2022 - now 93% of their labels are clear. Walgreens? Only 38%. Independent pharmacies? Just 28%.
Units That Can Kill: mL vs. Teaspoons
For liquid medicines, the unit of measure can be life-or-death. If your label says "Take 1 teaspoon," you might grab a kitchen spoon. But kitchen spoons vary wildly. One might hold 4 mL, another 7 mL. That’s nearly double the dose.
The FDA and U.S. Pharmacopeia have required for years that all liquid prescriptions use milliliters (mL) - not teaspoons or tablespoons. Yet in 2021, an FDA audit found 63.8% of liquid medication labels still used non-standard units. That’s over half of all prescriptions.
NIH research showed patients using teaspoons made measurement errors 27.4% of the time. That’s nearly 1 in 4 doses. The fix? Always use the dosing cup or syringe that comes with the medicine. Never guess with a kitchen spoon. And if your label says "1 tsp," ask your pharmacist to rewrite it in mL - it’s your right.
"As Needed" Doesn’t Mean "Whenever You Feel Like It"
"Take as needed for pain" is one of the most misunderstood instructions. People think it means they can take it whenever they want. But most pain meds have a daily limit. Tylenol (acetaminophen) can cause liver damage if you take more than 4,000 mg in 24 hours. That’s about eight 500 mg pills.
A Consumer Reports survey found 67.8% of people didn’t know the maximum daily dose for their "as needed" pain medication. That’s terrifying. If your label says "Take 1 tablet every 6 hours as needed," that means up to four times a day - not six, not eight. Always check the maximum daily dose on the bottle or ask your pharmacist.
Same goes for sleep aids, anxiety meds, or muscle relaxants labeled "as needed." They’re not free passes. Overuse can lead to dependence, dizziness, or worse.
Timing Matters More Than You Think
Some medications need to be taken on an empty stomach. Levothyroxine, for thyroid treatment, is a classic example. If you take it with coffee, food, or calcium supplements, your body absorbs less of it - and your thyroid levels stay off. The FDA-approved label says "take on an empty stomach, 30 to 60 minutes before breakfast." But a Harvard Health survey found 32.7% of patients took it with food anyway.
Other drugs need food to reduce stomach upset. Metformin for diabetes? Taking it with meals cuts nausea by half. A patient on PatientsLikeMe said switching from "Take 2 tablets daily" to "Take 1 with breakfast and 1 with dinner" made their stomach feel better almost immediately.
For cancer drugs or heart medications with narrow therapeutic windows, timing is even more precise. Some labels now say: "Take between 8:00 a.m. and 10:00 a.m." That’s not a suggestion - it’s medical necessity.
What About Night Shift Workers?
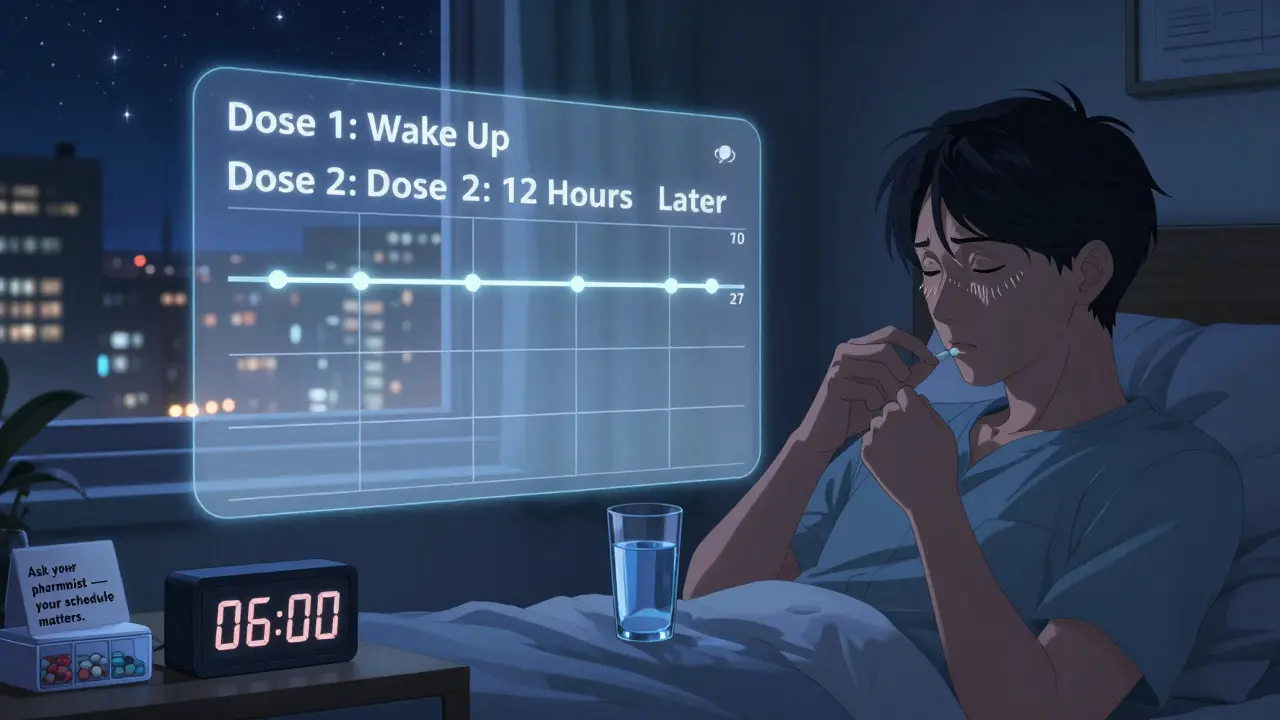
Here’s a real-world problem: what if you work nights? If your label says "Take in the morning and evening," what does that mean for you? "Morning" might be 10 p.m. for you, and "evening" might be 6 a.m.
Dr. Michael Wolf’s 2022 study found 22.3% of night-shift workers got confused by standard timing labels. They took their morning dose at 7 a.m. - right before bed - and missed the evening dose entirely.
The solution? Talk to your pharmacist. Ask: "What’s the best way to space these doses based on my schedule?" You might get: "Take one when you wake up and one 12 hours later." That’s flexible, safe, and personalized.
What Those Weird Abbreviations Really Mean
You’ll see things like "b.i.d.", "t.i.d.", or "q.d." on older labels. These are Latin abbreviations. But only 37.4% of patients understand them, according to the American Medical Association.
- b.i.d. = twice daily
- t.i.d. = three times daily
- q.d. = once daily
- q.i.d. = four times daily
- q4h = every 4 hours
Don’t guess. If you see these, ask your pharmacist to write it out in plain English. Most pharmacies are required to do this now - especially if you have low health literacy. The AMA says plain language reduces errors by over 50%.
What You Can Do Right Now
Here’s your action plan - simple, practical, and life-saving:
- Read the label. If it says "twice daily," ask: "What times?"
- For liquids, check the unit. If it says "teaspoon," ask for a new label in mL.
- For "as needed" meds, find the maximum daily dose. Write it down.
- If you work nights, tell your pharmacist your schedule. Ask for a custom timing plan.
- Don’t trust abbreviations. Ask for plain English.
- Use a pill organizer with time slots. Set phone alarms if needed.
Pharmacists are trained to help you with this. But they can’t read your mind. You have to speak up.
What’s Changing in 2025 and Beyond
The system is getting better - slowly. By January 1, 2027, the FDA plans to require every prescription label to include a "Medication Schedule Grid" - a simple chart showing exactly when to take each dose each day. Think of it like a weekly calendar for your pills.
Some pharmacies are already testing augmented reality labels. Point your phone at the bottle, and a video shows you how and when to take the medicine. Early tests show a 52.3% drop in timing errors.
And by 2026, the U.S. government wants 90% of pharmacies to use clear, explicit timing instructions. That’s a big shift - and it’s coming fast.
Final Thought: Your Safety Is Your Responsibility
Medication errors aren’t always the pharmacist’s fault. They’re not always the doctor’s fault. Sometimes, they’re just the result of unclear labels and quiet confusion.
You have the right to understand your medicine. You have the right to ask questions. And you have the power to prevent harm - just by reading the label, asking for clarity, and speaking up when something doesn’t make sense.
Don’t assume. Don’t guess. Ask.
What does "twice daily" really mean on a prescription?
"Twice daily" means two doses in a 24-hour period, but it doesn’t say when. For safety, it should be clarified as "Take one in the morning and one in the evening." If your label doesn’t specify times, ask your pharmacist to write it out clearly. Timing affects how well the medicine works and whether you avoid side effects.
Can I use a kitchen spoon to measure liquid medicine?
No. Kitchen spoons vary in size and can lead to dangerous overdoses or underdoses. Always use the dosing cup, syringe, or dropper that comes with the medicine. The FDA requires all liquid prescriptions to list doses in milliliters (mL), not teaspoons. If your label still says "teaspoon," ask for a corrected label.
What should I do if my prescription says "as needed"?
"As needed" doesn’t mean "whenever you want." There’s always a maximum daily dose. For example, acetaminophen (Tylenol) should not exceed 4,000 mg in 24 hours. Check the bottle or ask your pharmacist for the limit. Never exceed it - even if you’re still in pain. Overdosing can cause liver damage or other serious harm.
Why does my pill say "take on an empty stomach"?
Some medications, like levothyroxine or certain antibiotics, won’t absorb properly if taken with food, coffee, or supplements. Taking them on an empty stomach means 30 to 60 minutes before eating. If you’re unsure, ask your pharmacist what to avoid. Ignoring this can make your medicine less effective.
I work nights. How do I take my medicine if the label says "morning and evening"?
"Morning" and "evening" are based on a typical day. If you work nights, ask your pharmacist to adjust the timing to match your schedule. For example: "Take one when you wake up and one 12 hours later." This keeps the doses spaced evenly without forcing you to take them at times that don’t fit your life.
What do "b.i.d." and "t.i.d." mean on my prescription?
"b.i.d." means twice daily. "t.i.d." means three times daily. These are Latin abbreviations, and most people don’t understand them. The American Medical Association recommends avoiding them entirely. Ask your pharmacist to rewrite the instructions in plain English: "Take two tablets a day" or "Take one tablet three times a day."


13 Responses
I had no idea kitchen spoons could be so dangerous. I’ve been measuring my kid’s antibiotics with a regular spoon for years. Just got back from the pharmacy and they rewrote my label in mL. I’m crying. This is life-saving info.
Of course the FDA cares about this now. They only act after someone dies. Meanwhile, my pharmacy still prints ‘b.i.d.’ like it’s 1998. If they can’t even spell ‘twice daily’ right, why should I trust them with my life?
You people are overreacting. I’ve been taking my meds ‘twice daily’ for 15 years and I’m fine. The real problem is people who can’t follow basic instructions. Stop blaming the label and start taking responsibility.
It is, indeed, a matter of considerable concern that the prevailing nomenclature employed on pharmaceutical labels remains regrettably archaic. The linguistic ambiguity inherent in such terms as ‘b.i.d.’ and ‘t.i.d.’ constitutes a significant impediment to therapeutic adherence, particularly among populations with limited health literacy. A standardized, unambiguous lexicon is not merely advisable-it is an ethical imperative.
Bro, I work night shift in Mumbai and this post saved my life. My doc said 'take 2x daily' and I was taking it at 7am and 7pm. Now I take it when I wake up (3pm) and 12hrs later (3am). No more dizziness. Also, always use the syringe. Kitchen spoon = bad. 1 tsp = 5mL but your spoon? Maybe 8mL. You don't wanna be that guy.
I’ve been telling my mates this for years. If your label says ‘teaspoon’, you’re already losing. Just use the bloody syringe.
This is all a government scam to make us buy more syringes and pill organizers. They don’t want us to be healthy. They want us dependent. And why are they pushing AR labels? Are they spying on us when we take our meds? I’m not falling for it.
The fact that 82.7% of pharmacies still use outdated terminology speaks volumes about systemic negligence in healthcare communication. It’s not just poor labeling-it’s a failure of institutional empathy. I’ve had to educate my own pharmacist. Twice.
In my family in Colombia, we always ask the pharmacist to write the times in our own language-‘en la mañana’ and ‘en la noche’. It’s not just about clarity, it’s about dignity. Medicine should speak to you, not over you. And yes, I use a pill box with pictures. My abuela taught me that.
The true tragedy here isn’t the label-it’s the erosion of trust. We’ve been conditioned to accept ambiguity as normal. We don’t question because we’ve been taught that expertise is sacred, not serviceable. But health isn’t a hierarchy-it’s a conversation. And if your pharmacist won’t speak plainly, you’re not being irresponsible-you’re being silenced.
I read this and thought ‘finally’-then I checked my last prescription. Still says ‘b.i.d.’. And guess what? My pharmacist laughed when I asked. So no, this isn’t about education. It’s about laziness. And corporate cost-cutting. The system doesn’t care if you live or die, as long as you keep buying pills.
I’m a nurse and I’ve seen people mix up their insulin with their blood pressure meds because the labels looked too similar. This isn’t just about wording-it’s about design. Labels need color coding, icons, spacing. We’re not just reading words-we’re navigating risk.
I’ve been taking levothyroxine for 8 years. I take it at 7am with a glass of water. No coffee. No food. No calcium. I used to forget. Now I have a little alarm that says ‘thyroid time’. It’s weirdly comforting.