When you’re breastfeeding and need to take a medication, it’s natural to wonder: is this going to hurt my baby? You’re not alone. Nearly one in two mothers stops breastfeeding earlier than they want to because they’re worried about what’s in their milk. But here’s the truth most doctors don’t tell you: 98% of medications are safe to take while breastfeeding. The real issue isn’t the drugs themselves-it’s the confusion around how they move into milk, how much your baby actually gets, and what really matters for their safety.
How Do Medications Even Get Into Breast Milk?
Breast milk isn’t just filtered blood. It’s made inside tiny sacs in the breast called alveoli, lined with cells that pull substances from nearby capillaries. Most drugs cross into milk the same way water does-through passive diffusion. That means they follow a simple rule: they move from where there’s more of them (your bloodstream) to where there’s less (your milk), until levels balance out.
That’s why small, fat-soluble drugs cross easily. Think of diazepam (Valium) or sertraline (Zoloft). These molecules are light-under 300 daltons-and slip through cell membranes like oil through a sieve. On the flip side, big drugs like heparin (15,000 daltons) or insulin (5,800 daltons) barely make it through. They’re too large. Your baby gets almost nothing.
There’s also a trick called ion trapping. If a drug is a weak base-like amitriptyline or pseudoephedrine-and your milk is slightly more acidic than your blood (which it usually is), the drug gets ‘trapped’ in the milk. That’s why some antidepressants show up in milk at 2 to 5 times the concentration in your blood. It’s not because your body is dumping toxins-it’s chemistry.
And don’t forget timing. Right after birth, your breast cells are still loosely connected. Between days 4 and 10, even larger molecules can slip through. After that, those gaps close. So if you take a medication early on, your baby might get a slightly higher dose than if you started a week later.
How Much Actually Reaches Your Baby?
Here’s where most people panic for no reason. Even when a drug shows up in milk, your baby doesn’t absorb it all. Their gut isn’t fully developed. Their liver is tiny. And most drugs are broken down before they ever enter the bloodstream.
Take amoxicillin, a common antibiotic. Your milk might have 1.5% of your dose in it. But your baby swallows only a few milliliters at a time. Their total exposure? About 0.1% to 0.5% of your weight-adjusted dose. That’s less than what they’d get from a single drop of liquid medicine. And it’s not enough to cause harm.
Even with stronger drugs, the numbers are reassuring. For diazepam, your baby might get up to 7% of your dose-but because it’s stored in fat and released slowly, it doesn’t build up dangerously in a healthy term infant. The real risk comes with premature babies or those with liver problems. Their systems can’t clear drugs as fast. That’s why doctors watch them more closely.
For antidepressants like sertraline, infant serum levels are typically 1-2% of the mother’s level. That’s below the threshold for clinical effect. In fact, studies show babies exposed to sertraline through breast milk have no increased risk of developmental delays, sleep issues, or behavioral problems compared to unexposed babies.
What Medications Are Actually Dangerous?
Let’s cut through the noise. There are only a handful of drugs you need to avoid. And they’re not the ones you think.
Radioactive iodine (I-131) is one. It goes straight to the thyroid. If you’re getting a scan or treatment for thyroid cancer, you’ll need to stop breastfeeding for weeks. No way around it.
Chemotherapy drugs like methotrexate or cyclophosphamide are another. They’re designed to kill fast-growing cells-and that includes your baby’s developing tissues. These are clear no-gos.
High-dose estrogen birth control (over 50 mcg ethinyl estradiol) isn’t toxic to babies-but it can shut down your milk supply in as little as 72 hours. That’s why progestin-only pills are the go-to for breastfeeding moms.
Bromocriptine (used to dry up milk) is another. It works by crushing prolactin. If you’re trying to breastfeed, don’t take it.
Everything else? Most antibiotics, painkillers like ibuprofen and acetaminophen, blood pressure meds, thyroid pills, and even most antidepressants? Safe. The American Academy of Pediatrics says 87% of commonly used drugs fall into the ‘usually compatible’ category. That’s not a guess. That’s data from 2,500+ drugs tracked by the InfantRisk Center since 2006.
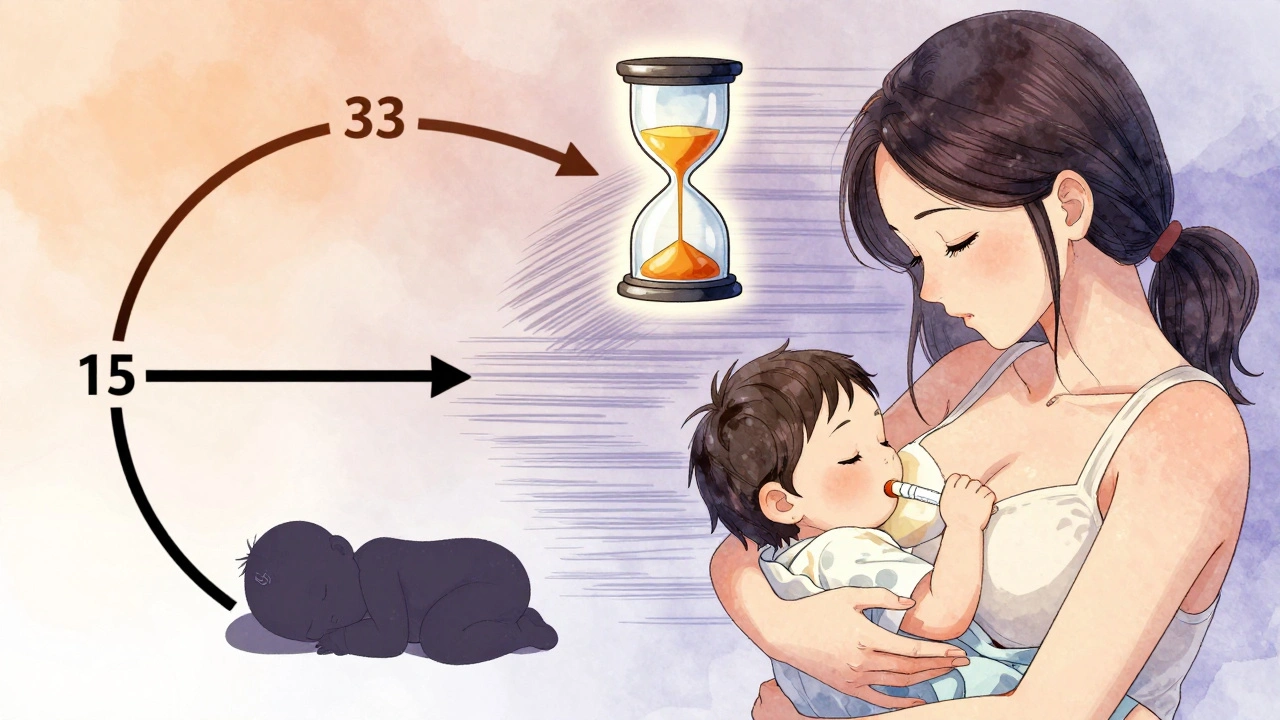
Timing Matters More Than You Think
When you take your pill can make a bigger difference than which pill you take.
Take your medication right after you breastfeed. That gives your body time to break down and clear the drug before the next feeding. For most drugs, peak blood levels happen 1-2 hours after ingestion. Waiting 3-4 hours before the next feed can reduce your baby’s exposure by 30-50%.
For long-acting drugs like diazepam or fluoxetine, this matters even more. Diazepam stays in your system for days. If you take it right before a feeding, your baby gets hit with the full dose. If you take it after feeding, they get a trickle.
And if you’re on a medication with a long half-life in babies-like phenobarbital-your doctor might ask you to space doses or check your baby’s blood levels. That’s rare, but it happens when the risk is higher.
What Should You Watch For in Your Baby?
Most babies show zero signs. But if you’re taking a psychotropic drug, an opioid, or something that affects the nervous system, keep an eye out for:
- Excessive sleepiness or difficulty waking for feeds
- Poor feeding or sucking weakness
- Unusual fussiness or jitteriness
- Diarrhea or vomiting
These signs are rare. In fact, a 2022 study found only 8.7% of babies exposed to SSRIs showed mild irritability-and most of those cases resolved on their own. Only 5.3% had trouble feeding. And in almost all cases, switching to a different drug or adjusting timing fixed it.
Don’t panic if your baby seems a little sleepy after you take a painkiller. That’s normal. But if they’re sleeping through three feeds in a row, call your pediatrician. That’s a red flag.
What About Supplements, Herbs, and CBD?
Just because something is ‘natural’ doesn’t mean it’s safe in breast milk.
Herbs like sage and peppermint can reduce milk supply. CBD? We don’t have good data. The FDA warns against it because it can build up in fat tissue and may affect brain development. Melatonin? Some moms use it for sleep, but infant exposure isn’t well studied. Stick to what’s been tested.
And never take anything recommended by a stranger online. A 2022 study found 12.7% of breastfeeding women took medications or supplements that were contraindicated based on official guidelines. Most didn’t know.
What’s the Bottom Line?
You don’t have to choose between being a healthy mom and being a breastfeeding mom. Almost every medication you need is safe to take while breastfeeding. The real danger isn’t the drugs-it’s stopping breastfeeding out of fear.
Here’s what to do:
- Don’t stop your meds without talking to your doctor. Untreated depression, high blood pressure, or infection can hurt you-and your baby-more than the drug.
- Take your medication right after feeding, not before.
- Watch your baby for signs of drowsiness, poor feeding, or irritability.
- Use trusted resources like the InfantRisk Center or LactMed app (version 3.2 or later) to check your specific drug.
- If you’re unsure, ask your pediatrician or a lactation consultant. Don’t rely on Google.
Over 80% of mothers in the U.S. start breastfeeding. That’s powerful. Don’t let misinformation make you quit before you need to. With the right info, you can take care of yourself and still give your baby the best start.


8 Responses
I wish more doctors would say this out loud. I was terrified to take my antidepressant after my son was born, so I stopped breastfeeding for three weeks. Turned out he was fine, but I was a mess. My milk dried up, and I felt like I failed. This post is the kind of info I needed back then.
Let’s be real - if you’re taking SSRIs and still breastfeeding, you’re basically gambling with your kid’s neurodevelopment. The AAP says ‘usually compatible’? That’s not safety, that’s corporate liability language. The FDA hasn’t approved any antidepressants for lactation. Don’t be fooled by cherry-picked stats.
There’s a beautiful symmetry here: biology doesn’t judge intention. The body doesn’t care if you’re taking medication because you’re depressed, hypertensive, or diabetic - it just moves molecules according to physics and chemistry. The fear isn’t in the drug; it’s in the story we tell ourselves about motherhood and purity. You’re not poisoning your child. You’re sustaining them, even when you’re broken.
so like… if i take cbd gummies for my anxiety and my baby gets a lil sleepy… is that just ‘normal’?? or am i just a bad mom who thinks ‘natural’ means ‘no consequences’?? 😅
Timing matters more than most people realize. I took ibuprofen right after nursing for months - my daughter never even blinked. But when I accidentally took it before a feed? She slept for five hours straight. That’s not coincidence. That’s pharmacokinetics. Do the math. Don’t guess.
As a mom from a culture where breastfeeding past a year is normal, I’m tired of the Western fear-mongering. My grandmother breastfed five kids while working in the fields, taking herbal teas and painkillers without a single concern. We didn’t have apps or studies - we had community. Trust your instincts, not your algorithm.
While I appreciate the sentiment expressed in this article, I must emphasize that the American Academy of Pediatrics’ classification of ‘usually compatible’ lacks the rigor of a formal FDA labeling system. The absence of contraindications does not equate to affirmation of safety. I urge all lactating individuals to consult their prescribing physician and request a pharmacokinetic risk assessment prior to medication administration.
My sister stopped breastfeeding because she was told ‘avoid all meds’ - then she had a breakdown. She’s on sertraline now, and her daughter is thriving. The real danger isn’t the pill. It’s the silence. Thank you for speaking up. This is the kind of truth that saves families.