Hemolytic Anemia Risk Assessment Tool
Medication Risk Assessment
This tool helps identify potential drug-induced hemolytic anemia risk based on your medications, symptoms, and timing. NEVER delay seeking medical care if you suspect hemolytic anemia - this is not a substitute for professional medical diagnosis.
URGENT: Stop this medication immediately if you have high-risk symptoms. This is a medical emergency.
Always consult your healthcare provider for proper diagnosis and treatment. This assessment tool is for informational purposes only and does not replace medical advice.
When you take a medication, you expect it to help - not break down your own blood. But for some people, common drugs can trigger a dangerous chain reaction: the immune system starts attacking red blood cells, destroying them before they’ve done their job. This isn’t a rare glitch. It’s drug-induced immune hemolytic anemia (DIIHA), a real and often missed medical emergency that can turn a simple antibiotic into a life-threatening trigger.
How a Drug Turns Against Your Blood
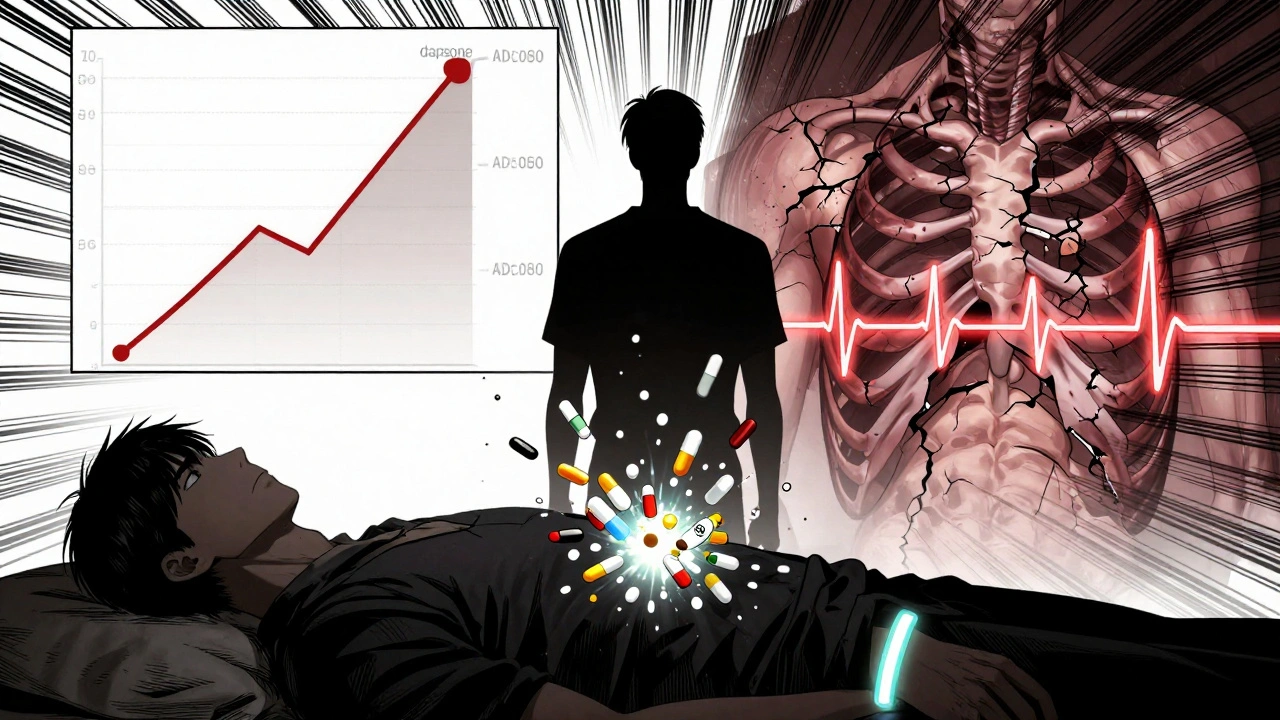
Your red blood cells live for about 120 days. They carry oxygen, then get quietly recycled. But when certain drugs enter the picture, they can stick to the surface of these cells like unwanted stickers. The immune system sees these drug-coated cells as foreign invaders and sends antibodies to destroy them. This is immune-mediated DIIHA. It’s not an allergy - it’s a mistaken identity crisis inside your bloodstream. The most common culprits? Cephalosporin antibiotics, especially cefotetan, ceftriaxone, and piperacillin. Together, they cause about 70% of immune-mediated cases. Other drugs like methyldopa, levodopa, and even NSAIDs like ibuprofen can also trigger this reaction. The timing matters: symptoms usually appear after 7 to 10 days of continuous use. That’s why it’s easy to miss - doctors and patients often assume the problem is something else. Then there’s oxidative hemolysis. This version doesn’t involve antibodies. Instead, the drug directly damages hemoglobin inside red blood cells, turning it into clumps called Heinz bodies. This mostly happens in people with G6PD deficiency - a genetic condition affecting 10-14% of African American men and 4-15% of people of Mediterranean descent. But even if you don’t know you have it, drugs like dapsone, phenazopyridine (Pyridium), ribavirin, and benzocaine can still cause rapid red blood cell destruction within 24 to 72 hours.What You’ll Feel - And What Doctors Look For
The symptoms are broad and easily confused with the flu, exhaustion, or a bad cold. Fatigue hits 92% of patients. Weakness? 87%. Shortness of breath? 76%. Your heart races because your body is trying to compensate for the lack of oxygen. Skin turns pale. The whites of your eyes and your skin may yellow - that’s jaundice, caused by the breakdown of hemoglobin into bilirubin. But here’s the catch: these signs don’t show up on a basic blood test. You need specific lab markers to confirm hemolysis:- High indirect bilirubin (over 3 mg/dL)
- Elevated LDH (above 250 U/L)
- Low haptoglobin (under 25 mg/dL)
- Spherocytes or Heinz bodies on a blood smear
Who’s at Risk - And Why It’s Often Missed
G6PD deficiency is the biggest hidden risk factor. Many people never know they have it until they take a drug like sulfa antibiotics or antimalarials and suddenly collapse with dark urine and extreme fatigue. Even one dose can trigger a crisis. Children rarely get DIIHA - but when they do, it’s often more severe. One 2023 study found pediatric patients averaged a hemoglobin level of 5.2 g/dL, compared to 6.8 g/dL in adults. That’s critically low. And because kids don’t always describe symptoms clearly, delays in diagnosis are common. Even trained doctors miss this. A 2024 study showed internal medicine residents correctly diagnosed DIIHA in only 58% of cases on first review. After targeted training on drug triggers and lab patterns, that jumped to 89%. The problem? Many assume anemia means iron deficiency or blood loss - not drug-induced destruction.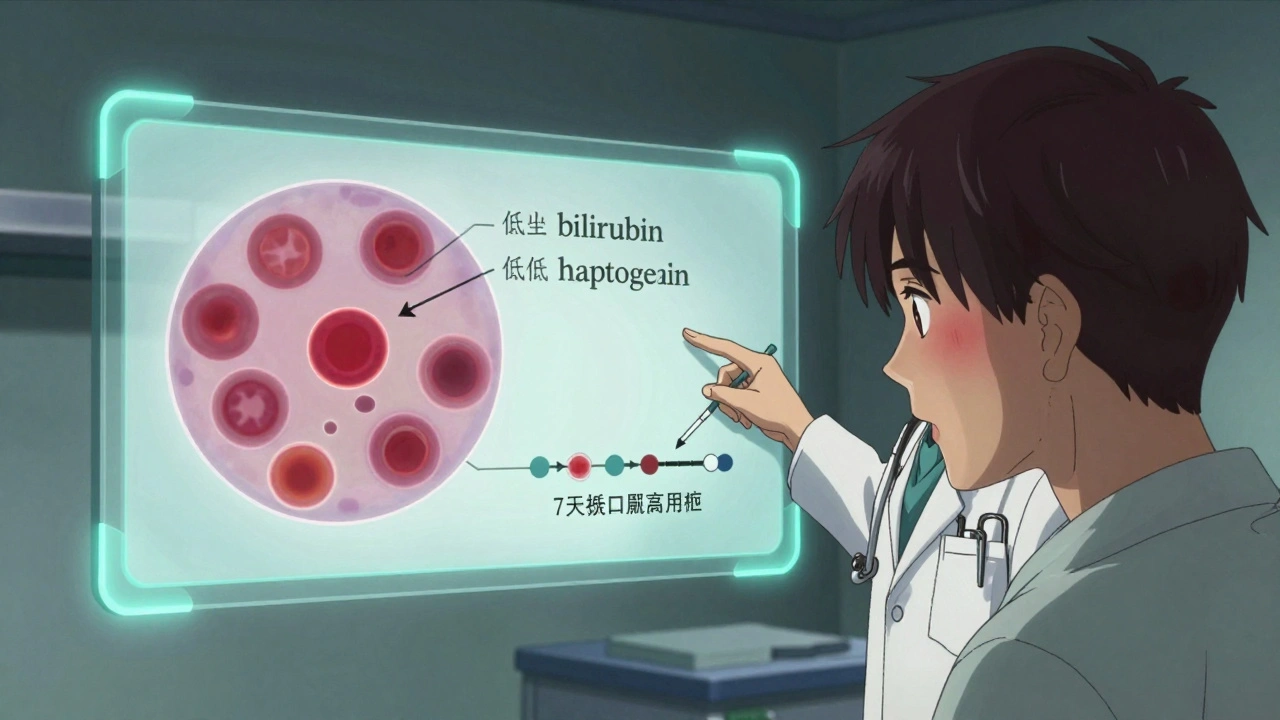
What to Do Immediately - And What Not to Do
The single most important step? Stop the drug. Right now. No waiting. No second opinions. If you suspect DIIHA, discontinue the medication immediately. That alone leads to stabilization in 95% of cases within 7-10 days, with full recovery in 4-6 weeks. If your hemoglobin drops below 7-8 g/dL or you’re dizzy, short of breath, or your heart is racing, you’ll likely need a blood transfusion. But transfusions aren’t always simple - antibodies can attack the donor cells too. That’s why blood banks must carefully match and screen. Here’s what you must avoid:- Methylene blue - used to treat severe methemoglobinemia - is deadly if you have G6PD deficiency. It can trigger massive hemolysis.
- Corticosteroids like prednisone are sometimes used, but their benefit is unclear. Most patients recover without them once the drug is stopped.
- Continuing the drug - even a single extra dose can push you into heart failure.
When It Gets Serious - And How It’s Treated
In rare cases, the immune system keeps attacking even after the drug is gone. That’s called drug-independent autoantibody activity. When that happens, treatment escalates:- Intravenous immunoglobulin (IVIG) - 1 g/kg per day for two days - helps calm the immune response.
- Rituximab - a monoclonal antibody - given weekly for four weeks, shuts down the antibody-producing cells.
- Azathioprine or cyclosporine - longer-term immunosuppressants for stubborn cases.
Prevention Is Possible
Hospitals that added drug-hemolysis alerts to their electronic health records saw a 32% drop in severe DIIHA cases over 18 months. That’s proof that awareness saves lives. If you’ve ever had unexplained anemia after starting a new medication, tell your doctor. List every drug you’ve taken - including over-the-counter ones like ibuprofen or topical benzocaine sprays. If you’re of African or Mediterranean descent, ask about G6PD testing - even if you’ve never had symptoms. It’s a simple blood test that can prevent a crisis. And if you’re prescribed a cephalosporin, dapsone, or phenazopyridine - especially if you’ve had anemia before - ask: “Could this cause red blood cell destruction?” Most doctors won’t bring it up. But if you ask, you might just save your life.What Happens After Recovery?
Once you recover, you’ll need to avoid the drug that caused the problem - forever. Cross-reactivity is real. If ceftriaxone triggered your hemolysis, you can’t safely take other cephalosporins. Even penicillin derivatives can be risky. If you had oxidative hemolysis and tested negative for G6PD during the acute episode, get tested again in 2-3 months. During active hemolysis, the test can give false negatives because it measures enzyme levels in older red blood cells - and those are the ones being destroyed. Newer cells, with normal G6PD, will show up later. Keep a list of all drugs that caused problems. Share it with every new doctor. Wear a medical alert bracelet if you have G6PD deficiency. And remember: if you feel suddenly tired, short of breath, or notice yellowing skin after starting a new pill - don’t wait. Get checked. Hemolytic anemia doesn’t always come with warning signs. But it always responds to fast action.Can over-the-counter drugs cause hemolytic anemia?
Yes. Even common OTC drugs like ibuprofen and naproxen (NSAIDs) have been linked to immune-mediated hemolytic anemia. Topical benzocaine, found in throat sprays and teething gels, can trigger oxidative hemolysis - especially in people with undiagnosed G6PD deficiency. Never assume a drug is too mild to cause harm.
How long does it take to recover from drug-induced hemolytic anemia?
Most people start improving within 7-10 days after stopping the drug. Hemoglobin levels typically return to normal in 4-6 weeks. Recovery is faster in younger, healthier people. If complications like heart strain or persistent antibodies occur, recovery may take longer and require additional treatment.
Is hemolytic anemia from drugs common?
No - it’s rare. But it’s serious. While only a few cases occur per 100,000 drug prescriptions, it’s one of the most dangerous drug reactions because it can escalate quickly. The rarity makes it easy to miss, which is why awareness matters.
Can you get DIIHA from a single dose of a drug?
For immune-mediated DIIHA, usually not. It takes 7-10 days of exposure for the immune system to build antibodies. But for oxidative hemolysis - especially in G6PD-deficient people - a single dose of drugs like dapsone or phenazopyridine can cause rapid, severe destruction within 24-72 hours.
Does having hemolytic anemia once mean you’ll get it again?
Not from other drugs - but you’re at high risk if you’re exposed to the same drug again. Once your immune system has made antibodies to a specific drug, even a tiny amount can trigger a fast, severe reaction. Avoidance is the only reliable prevention.


12 Responses
This is why I don't trust big pharma. They sell you pills like candy and then act shocked when you start dying. 🤡
People still don't realize NSAIDs can kill your RBCs. Ibuprofen isn't harmless. Stop treating it like water.
Of course they missed this. The medical system is designed to ignore rare side effects until someone dies. Then they write a paper and move on.
so like... benzocaine in teething gel can wreck your blood?? like. wow. i had no idea. my cousin used that on her kid and she got super pale. we thought it was just a virus lol
This raises a deeper question: why do we assume safety in familiarity? Just because a drug is OTC or widely prescribed doesn't mean it's benign. The body doesn't care about regulatory status. It responds to chemistry. And we're still treating pharmacology like it's a moral issue rather than a biological one.
The clinical data presented herein is both compelling and concerning. It is imperative that healthcare professionals incorporate a more rigorous pharmacovigilance framework into routine practice, particularly with regard to the temporal association between drug administration and haematological derangements.
I can't believe people still don't get this. You take a drug, your body turns on itself, and then you blame the patient for not 'knowing better'? That's not medicine, that's negligence. I've seen it happen. It's not rare. It's just hidden.
You ever wonder if this is all a cover-up? The FDA knows. The drug companies know. They let these drugs stay on the market because they make too much money. And then they blame G6PD deficiency like it's the patient's fault for existing.
I'm not surprised. People who can't afford genetic testing are just supposed to die quietly? This isn't medicine, it's class warfare dressed in white coats. You need money to know you're at risk.
I mean... I get it, but... how many people actually die from this? Like, is it really worth the panic? I've taken ceftriaxone three times. Still here.
If you're of African or Mediterranean descent and have ever experienced unexplained fatigue after taking a new medication, get tested for G6PD deficiency. It's a simple, inexpensive test that can prevent a life-threatening event. This isn't fearmongering - it's preventive care. And if you're a clinician, don't wait for symptoms to be 'classic.' Ask the question before prescribing.
Stop the drug. Get checked. Don't wait.