If you’ve ever woken up with a burning chest or a sour taste in your mouth, you’re not alone. About 20% of adults in the U.S. deal with GERD symptoms at least once a week. For many, it starts as occasional heartburn after a big meal - but when it happens twice a week or more, it’s no longer just indigestion. It’s gastroesophageal reflux disease, or GERD. And while pills like omeprazole or esomeprazole (PPIs) can bring quick relief, they’re not the whole story. The real key to lasting control? Combining medication with real, sustainable lifestyle changes.
What’s Actually Happening in Your Body?
GERD isn’t just “too much acid.” It’s a broken valve. The lower esophageal sphincter (LES), a ring of muscle at the bottom of your esophagus, should open to let food into your stomach and then shut tight. In GERD, it loosens at the wrong times. That lets stomach acid - which can be as strong as pH 1.5 - splash back up into your esophagus. Your stomach lining is built to handle that. Your esophagus isn’t. That’s what causes the burn, the cough, the hoarseness, even the bad breath. Symptoms vary. Some people get classic heartburn. Others never feel chest pain at all. Instead, they have a chronic cough, a sore throat that won’t go away, or feel like something’s stuck in their throat. These are silent signs. And if left unchecked, GERD can lead to complications: strictures (narrowing of the esophagus), ulcers, or Barrett’s esophagus - a condition that increases the risk of esophageal cancer. That’s why treating it isn’t just about feeling better today. It’s about protecting your long-term health.PPIs: Powerful, But Not a Permanent Fix
Proton pump inhibitors - drugs like omeprazole, pantoprazole, and esomeprazole - are the most effective acid-reducing medications available. They work by shutting down the acid-producing pumps in your stomach lining. Unlike antacids (which just neutralize acid temporarily) or H2 blockers (which reduce acid by about 60-70%), PPIs cut production by 90-98%. That’s why they heal erosive esophagitis in 70-90% of cases, compared to 50-60% with H2 blockers. But here’s the catch: PPIs don’t fix the broken valve. They just mask the symptom. And they come with risks if used too long. Studies show that taking PPIs for more than a year increases your risk of:- Enteric infections like Clostridium difficile (up to 50% higher risk)
- Vitamin B12 deficiency (because acid is needed to absorb it)
- Low magnesium levels, which can cause muscle cramps or irregular heartbeat
- Higher chance of hip fractures in older adults (35% increase with 3+ years of use)
Lifestyle Changes: The Real Game-Changer
Medication alone doesn’t cut it. The most effective approach is combining PPIs with lifestyle shifts - and the evidence is clear. Losing just 5-10% of your body weight can reduce GERD symptoms by half. That’s not magic. It’s physics. Extra belly fat pushes up on your stomach, forcing acid out. Here’s what actually works, based on patient data and clinical studies:- Stop eating 2-3 hours before bed. Lying down lets gravity stop working in your favor. Studies show this cuts nighttime acid exposure by 40-60%.
- Avoid trigger foods - but know your own. Coffee, tomatoes, alcohol, chocolate, and fatty foods trigger symptoms in 70-80% of people. But not everyone reacts the same. One person might be fine with spicy food. Another gets wrecked by citrus. Keep a food diary for 2 weeks. Note what you eat and when symptoms hit.
- Elevate the head of your bed. Raising it 6-8 inches with blocks or a wedge pillow keeps acid from flowing back while you sleep. Many patients report this single change eliminated their nighttime symptoms.
- Quit smoking. Smoking weakens the LES and reduces saliva production - and saliva helps neutralize acid. Smokers are twice as likely to develop GERD.
- Wear loose clothing. Tight belts or pants increase abdominal pressure, pushing acid upward.
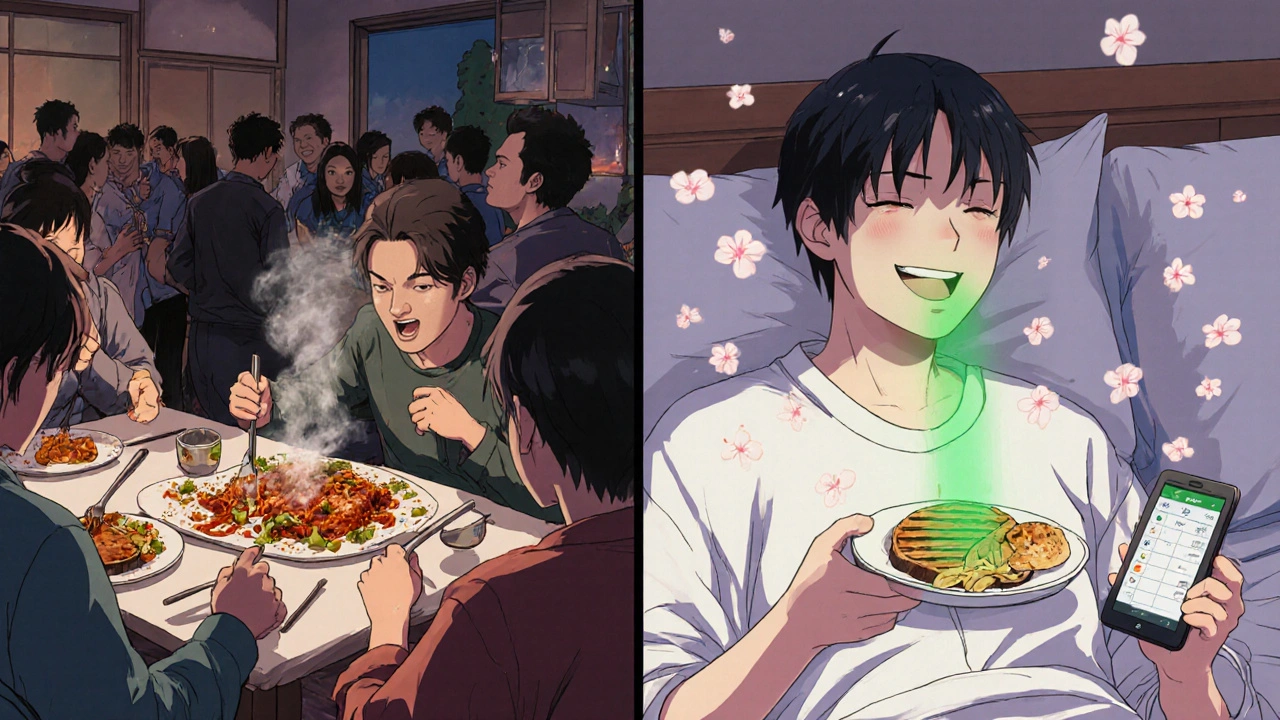
Why Most People Fail at Lifestyle Changes
You know what to do. But doing it? That’s the hard part. A Cleveland Clinic survey found 41% of patients struggled to stick with dietary changes because of social pressure - birthdays, dinners out, family traditions. It’s not laziness. It’s culture. Here’s how to make it work:- Plan ahead. Eat a light meal before going out. Order grilled chicken, steamed veggies, and water. Skip the fries and wine.
- Use apps like RefluxMD to track triggers. It’s rated 4.7/5 by over 8,500 users.
- Don’t go cold turkey. Cut out one trigger at a time. If coffee is your main issue, switch to decaf for two weeks. See how you feel.
- Enlist support. Tell your partner or friends you’re managing GERD. They can help you stick to your plan.
New Options Beyond PPIs
The GERD treatment landscape is changing. In 2023, the FDA approved Voquezna (vonoprazan), the first new acid-blocking drug class in 30 years. It works faster than PPIs and may have fewer long-term side effects. Early trials show 89% healing rates - slightly better than PPIs. For those who don’t respond to meds, there are minimally invasive procedures:- LinX® device: A small ring of magnetic beads is placed around the LES. It lets food through but snaps shut to block acid. 85% of users report symptom reduction at 5 years.
- TIF (Transoral Incisionless Fundoplication): A camera and tools are inserted through the mouth to rebuild the valve. 85% of patients say it improves quality of life more than PPIs after 2 years.

When to See a Doctor - Not Just a Pharmacist
If you’re using PPIs for more than 8 weeks without improvement, it’s time for an endoscopy. Same if you have:- Difficulty swallowing
- Unexplained weight loss
- Bloody or black stools
- Vomiting blood
Final Thought: It’s Not Either/Or
You don’t have to choose between pills and lifestyle. The best outcomes come from both. Start with lifestyle changes - they’re free, safe, and powerful. Use PPIs as a tool to give your esophagus time to heal, not as a lifelong crutch. Reevaluate every few months. Can you cut the dose? Try on-demand use? Go back to H2 blockers? The goal isn’t just to stop the burn. It’s to live without fear of the next episode. To eat without anxiety. To sleep through the night. That’s possible. But only if you treat the root cause - not just the symptom.Can I stop taking PPIs cold turkey?
No. Stopping PPIs suddenly can cause rebound acid hypersecretion, making your symptoms worse for weeks. Instead, work with your doctor to gradually reduce the dose over 4-8 weeks. You may switch to an H2 blocker like famotidine during the taper to help manage symptoms.
Do I need to avoid all acidic foods?
Not necessarily. It’s not about acidity - it’s about triggers. Tomatoes and citrus are common culprits, but not everyone reacts to them. The key is tracking. Keep a food diary for two weeks. Write down what you eat and when symptoms occur. Then eliminate the top 2-3 triggers one at a time. You might find you can still enjoy a small amount of lemon in your water.
Is GERD curable?
GERD isn’t usually “cured,” but it can be effectively managed - often without lifelong medication. Many people achieve long-term control through weight loss, dietary changes, and avoiding triggers. In some cases, procedures like LinX® or TIF can restore normal function. The goal is remission: no symptoms, no daily pills, no complications.
Can stress make GERD worse?
Yes. Stress doesn’t cause GERD, but it increases stomach acid production and makes you more sensitive to it. It can also lead to behaviors like late-night snacking or skipping meals - both of which trigger reflux. Managing stress through sleep, exercise, or mindfulness can reduce symptom frequency.
Are natural remedies like apple cider vinegar helpful?
There’s no solid evidence that apple cider vinegar helps GERD. In fact, vinegar is acidic and may irritate the esophagus further. Some people report feeling better, but that’s likely due to placebo or because they’re drinking it diluted and not on an empty stomach. Stick to proven methods: lifestyle changes, medication when needed, and medical supervision.
How long does it take to see results from lifestyle changes?
Most people notice improvement in 2-4 weeks, especially if they stop eating before bed and lose weight. But full healing of the esophagus can take 6-8 weeks. Be patient. Track your progress. Don’t expect overnight results - but don’t give up either. Consistency beats intensity.


9 Responses
Ugh, another post telling me to stop eating pizza and sleep upright like a mummy. I’ll stick with my PPIs, thanks.
While PPIs offer symptomatic relief, their long-term use correlates with micronutrient deficiencies-particularly B12 and magnesium-and alters gut microbiota composition significantly. The 2023 Johns Hopkins data on lifestyle interventions achieving 65% PPI discontinuation is compelling, yet underutilized in primary care. Consistency in dietary logging, sleep hygiene, and weight management remains the most evidence-based path to remission.
Let me tell you-this is the real MVP of health advice: stop eating at 9 p.m., elevate your bed, and lose 10 pounds. No magic pills. No snake oil. Just physics, discipline, and a little bit of courage to say ‘no’ to midnight tacos. I went from choking on acid every night to sleeping like a baby in 6 weeks. Not because I’m special-because I finally listened. Your esophagus isn’t a trash can. Treat it like the delicate, hardworking organ it is.
Modern medicine has reduced a complex physiological dysfunction-a neuromuscular failure of the LES-to a pharmacological Band-Aid, while society simultaneously glorifies convenience over bodily autonomy. We’ve outsourced our health to Big Pharma, then wonder why we’re chronically inflamed, vitamin-depleted, and emotionally exhausted. The real rebellion? Eating dinner before sunset. That’s not a lifestyle change-it’s a return to ancestral wisdom.
Guys-this isn’t just about acid. It’s about dignity. When you can’t sleep because your throat feels like it’s on fire, or you avoid hugs because you’re scared of burping? That’s not ‘normal.’ I tried everything-apple cider vinegar (don’t), baking soda (worse), and finally, I just stopped eating after 7 p.m. and raised my bed with cinderblocks. Three weeks later, I ate a slice of pizza without panic. It’s not easy. But it’s worth it. You’re not broken-you’re just misinformed.
pills are a scam the fda and big pharma made up to keep you buying them forever they dont even fix the valve they just make you feel better so you keep paying and the real cause is 5g of fluoride in your water i read it on a forum and the guy had a phd in chemistry so it must be true
Look, I get it. You want people to believe that lifestyle changes are the answer. But let’s be real-how many of us actually have the time, energy, or emotional bandwidth to track every bite, avoid every social gathering, and sleep in a wedge pillow like some kind of medieval monk? I work two jobs, have two kids, and my wife makes lasagna on Sundays. You’re asking me to give up my life for a 65% chance of feeling ‘better’? That’s not empowerment-that’s guilt wrapped in a clinical trial. And don’t even get me started on the LinX device. Sounds like a sci-fi horror movie.
Just wanted to say-this post saved me. I was on PPIs for 5 years. Felt like a zombie. Started logging food, stopped eating after 8, lost 12 lbs. Four weeks in, I cut my dose in half. Eight weeks? Off. No rebound. No panic. I still have a glass of wine sometimes. I still eat tomatoes. But I don’t eat them at midnight. It’s not perfection-it’s progress. You got this. Seriously. One small change at a time.
Thank you for the thorough and clinically grounded overview. The distinction between symptom suppression and physiological restoration is critical and often misunderstood. The data on Voquezna’s efficacy and the durability of TIF and LinX® procedures represent a paradigm shift in GERD management. However, access and cost remain significant barriers in underserved populations. I would encourage healthcare systems to integrate nutritional counseling and behavioral health support into routine GERD care-not as an adjunct, but as a foundational component. This is preventive medicine at its most humane.