Many people start taking fiber supplements to feel better-less bloating, regular bowel movements, lower cholesterol. But if you’re also on medication, you might be risking more than just an upset stomach. Fiber supplements can quietly interfere with how your body absorbs key drugs, turning your daily pills into less effective ones. It’s not about avoiding fiber. It’s about timing it right.
Why Fiber Interferes with Medications
Fiber doesn’t get digested. That’s why it works so well for digestion-it moves through your gut mostly unchanged. But that same quality makes it a silent thief of medication. When you swallow a fiber supplement like psyllium (Metamucil), methylcellulose (Citrucel), or even oat bran, those fibers can bind to drugs in your stomach and intestines. Think of it like a sponge soaking up liquid-but instead of water, it’s soaking up your pills. This binding happens through physical and chemical interactions. Some fibers have surfaces that attract drug molecules, holding them in place so they don’t get absorbed into your bloodstream. Others speed up how fast everything moves through your gut. If your medication doesn’t have enough time to be absorbed before it’s flushed out, you’re not getting the full dose. It’s not the same for every drug. Some medications are barely affected. Others? A small drop in absorption can mean big problems.Medications That Are Most at Risk
Certain drugs are especially sensitive to fiber interference because they need to be absorbed very precisely. Even a 10-20% drop in absorption can make them less effective-or even dangerous.- Levothyroxine (for hypothyroidism): Multiple studies show fiber reduces how much of this hormone your body absorbs. One study found patients taking levothyroxine with psyllium had higher LDL cholesterol levels-meaning their thyroid treatment wasn’t working as well. That’s not just inconvenient. It can lead to fatigue, weight gain, and heart problems over time.
- Metformin (for type 2 diabetes): Fiber can delay or reduce metformin absorption, which might cause blood sugar spikes. If you’re managing diabetes, that’s a serious risk.
- Lithium (for bipolar disorder): Lithium has a narrow therapeutic window. Too little, and mood swings return. Too much, and you risk toxicity. Fiber can alter how much enters your system, making dosage control harder.
- Olanzapine (for schizophrenia and bipolar disorder): Studies suggest fiber supplements may lower its absorption, potentially reducing its effectiveness.
- Carbamazepine (for seizures and nerve pain): Fiber can interfere with its absorption, increasing seizure risk if doses aren’t timed properly.
How Far Apart Should You Take Them?
The answer isn’t guesswork. Experts from Harvard Health, Mayo Clinic, and WebMD all agree: separate fiber supplements from medications by at least two hours. For some drugs, you need more.- For most medications: Take your fiber supplement at least 2 hours before or after your pill.
- For levothyroxine, lithium, or olanzapine: Wait 4 hours after taking your medication before taking fiber.
- For metformin: Take your fiber supplement at least 4 hours after your metformin dose.
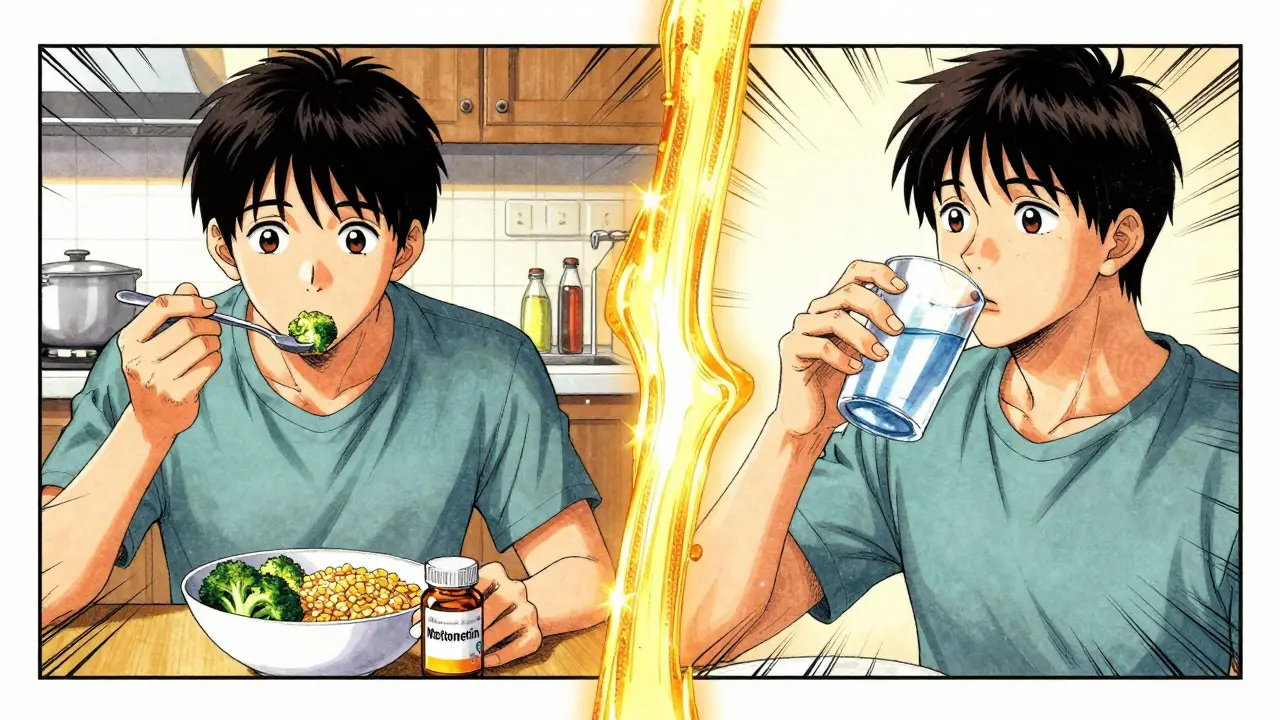
What About Fiber From Food?
You don’t need to stop eating broccoli, beans, or whole grains. Dietary fiber from food rarely causes problems because it’s mixed with other nutrients and digested more slowly. The real issue is concentrated fiber supplements. Think of it like this: eating a bowl of bran cereal with your pills is unlikely to interfere. Taking a spoonful of psyllium powder with them? That’s a different story. Still, if you’re eating a very high-fiber meal-think 20+ grams of fiber in one sitting-and you’re on a sensitive medication like levothyroxine, it’s safer to wait 2 hours after eating before taking your pill.How to Build a Safe Routine
Managing this isn’t about confusion. It’s about consistency.- Write down your meds and fiber schedule. Note what you take, when, and how much. Use a phone reminder or a paper log.
- Set alarms. If you take levothyroxine at 7 a.m., set a second alarm for 11 a.m. to take your fiber. Or vice versa.
- Take fiber with water. Always drink at least 8 ounces (240 ml) of water when you take a fiber supplement. Without enough liquid, it can swell in your throat and cause choking.
- Don’t take fiber before bed. It can cause bloating and gas that disrupt sleep. Take it earlier in the day.
- Check with your pharmacist. They know your full medication list and can flag high-risk combinations.


15 Responses
OMG YES THIS. I’ve been taking Metamucil with my levothyroxine for years and just last month my TSH spiked. My endo was like ‘did you change anything?’ and I was like ‘uhhh I just eat healthy?’ 😅 Thanks for spelling this out so clearly. I’m setting alarms now.
man i just take mine together and i’m fine. maybe i’m lucky?
you people are so naive. fiber supplements are just another corporate scam to sell you ‘wellness’ that’s barely regulated. the FDA doesn’t even require them to prove absorption interference. think about it. why do you think they don’t put warnings on the bottle? because they don’t want you to stop buying it. they’re making bank off your ignorance.
so… fiber is evil now? next you’ll tell me water interferes with meds. lol. if your meds are that fragile, maybe you shouldn’t be on them.
Let me just say-as someone who has read the actual pharmacokinetic studies (not just WebMD)-the real issue isn't fiber. It's the *formulation*. Psyllium’s gel-forming properties are uniquely problematic. Methylcellulose? Less so. And oat bran? Barely a blip. But no one wants to admit that the ‘fiber = good’ narrative is oversimplified. We’re being sold a myth. And now? We’re all just blindly following it. Sad.
Bro, I take fiber at 7am and my meds at 8pm. I’m basically a biohacker now. 🏆
in india we take fiber with medicine since 1990s no problem. you americans overthink everything
Bradly Draper says ‘maybe I’m lucky’? That’s not luck. That’s negligence. You’re not lucky-you’re a walking clinical trial waiting to go wrong. People die from underdosed lithium because someone thought ‘it’s fine.’ You’re not special. Your body isn’t magic. Stop pretending.
wait so if i eat a salad with my pills is that okay? i just want to know if i’m doing this wrong 😅
you think this is about fiber? nah. this is about the pharmaceutical industry controlling your body. they don’t want you to know that fiber can ‘detox’ your system naturally. they profit off your dependency. psyllium is a threat to their profits. that’s why they let you think it’s ‘safe’-until it’s too late. wake up.
is there a chart or something? like a printable one? i need to put it on my fridge 🥺
Thank you for this meticulously researched and clinically grounded exposition. The distinction between dietary fiber and concentrated supplements is both scientifically valid and critically undercommunicated in public health discourse. I shall be sharing this with my patients.
my grandma took fiber with her blood pressure meds for 30 years and she’s 92 and still gardening. just saying. 🌿
wait so i took my metformin and then 20 mins later had my fiber shake… is that bad? like… how bad? 😬
bro i take fiber at night and meds in morning. i think i got it figured out. also i dont trust doctors. they dont know shit. but i trust my gut. and my gut says this post is legit.