Drug-Induced Pulmonary Fibrosis Risk Assessment
This tool helps you assess your potential risk of developing drug-induced pulmonary fibrosis based on medications you're taking and other health factors. While this is not a medical diagnosis, it can help you identify when you should consult your doctor about potential risks.
Most people assume that if a doctor prescribes a medication, it’s safe. But some drugs quietly scar your lungs-long before you notice anything’s wrong. Drug-induced pulmonary fibrosis isn’t rare. It’s underdiagnosed, often mistaken for aging, asthma, or a lingering cold. And it can turn a routine treatment into a life-altering condition.
What Exactly Is Drug-Induced Pulmonary Fibrosis?
Pulmonary fibrosis means scar tissue builds up in your lungs. Think of it like internal scarring after a deep burn-but instead of skin, it’s the delicate walls of your air sacs (alveoli) that thicken and stiffen. When drugs cause this, it’s called drug-induced pulmonary fibrosis (DIPF). The lungs lose their ability to transfer oxygen into your blood. Breathing becomes harder, even at rest.
Unlike infections or asthma, this isn’t temporary swelling. It’s permanent damage. And the worst part? You might not feel it until it’s advanced. A dry cough, then shortness of breath during walks, then climbing stairs becomes impossible. By then, the scarring is often irreversible.
Which Medications Are Most Likely to Cause It?
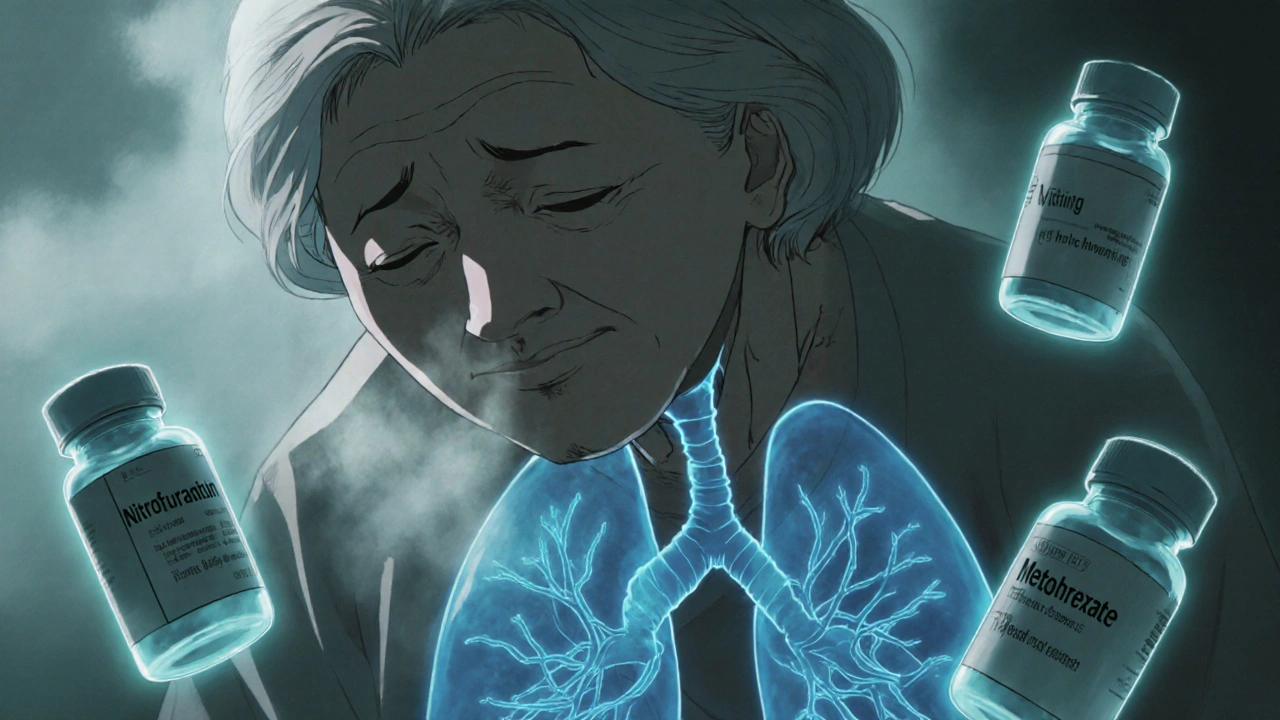
Over 50 medications have been linked to this condition. But only a handful account for most cases. Based on data from New Zealand’s pharmacovigilance system (2014-2024), three drugs stand out:
- Nitrofurantoin (used for UTIs): 47 reported cases. Often affects older adults on long-term low-dose therapy-sometimes after 6 months to 10 years. Symptoms appear slowly, so it’s easy to ignore.
- Methotrexate (for rheumatoid arthritis, psoriasis): 45 cases. Can trigger sudden, severe lung inflammation within weeks. Up to 7% of users develop it, especially if they’re over 60 or have existing lung issues.
- Amiodarone (for irregular heart rhythms): 39 cases. Takes months to years to show up. Risk spikes after taking more than 400 grams total-about 2-3 years of daily use. It’s one of the most common causes of fatal DIPF.
Chemotherapy drugs are another high-risk group:
- Bleomycin: Up to 20% of patients develop lung damage. Often happens after just a few doses. Doctors avoid it in people over 70 or with prior lung disease.
- Cyclophosphamide: Around 3-5% risk. Can cause both acute pneumonia and long-term scarring.
Even newer cancer drugs-immune checkpoint inhibitors like pembrolizumab and nivolumab-are now linked to DIPF. These drugs boost the immune system to fight tumors, but sometimes they turn it against the lungs. Cases have risen sharply since 2018.
Why Does This Happen? It’s Not About Dose
You might think, “I took it for years and never had a problem.” That’s true for most people. But for a small subset, it’s not about how much you take-it’s about your body’s reaction. It’s unpredictable.
Some people have genetic traits that make their lungs more vulnerable. Others develop a delayed immune response. The drug doesn’t just sit there-it breaks down into chemicals that trigger inflammation. Oxidative stress damages lung cells. Collagen piles up. Scar tissue forms. And once it’s there, it doesn’t go away.
That’s why two people on the same dose of amiodarone can have totally different outcomes. One stays fine. The other develops irreversible fibrosis. There’s no blood test to predict who’s at risk.
How Do You Know If It’s Happening to You?
Early symptoms are easy to brush off:
- A dry cough that won’t go away
- Getting winded faster than usual-walking to the mailbox, climbing stairs
- Feeling tired all the time, even after sleeping
- Unexplained weight loss or joint aches
Many patients wait months before seeing a doctor. One Reddit user from Manchester shared: “My GP said I was just getting older. I didn’t realize I was breathing through scar tissue until I collapsed during a walk.”
Diagnostic delays average 8.2 weeks. By then, lung function may have dropped by 30% or more. Doctors rely on three things:
- Your medication history-every pill you’ve taken in the last 12 months
- A high-resolution CT scan of your lungs-shows the telltale honeycomb pattern of scarring
- Ruling out everything else-infections, autoimmune disease, asbestos exposure
There’s no single test for DIPF. It’s a diagnosis of exclusion. That’s why telling your doctor every medication you’ve taken-even over-the-counter herbs-is critical.
What Happens If You Stop the Drug?
Stopping the offending medication is the single most important step. In 89% of cases, symptoms improve within 3 months if caught early.
But stopping isn’t always enough. If the scarring is advanced, doctors add:
- Corticosteroids (like prednisone): High doses for 2-4 weeks, then slowly tapered over 3-6 months. Reduces inflammation but comes with side effects-weight gain, mood swings, bone loss.
- Oxygen therapy: If your blood oxygen drops below 88%, you’ll need it at rest or during activity.
- Pulmonary rehab: Breathing exercises, physical conditioning, education. Helps you stay active despite reduced lung capacity.
Recovery isn’t guaranteed. About 75-85% of patients improve significantly. But 15-25% end up with permanent lung damage. A few die-especially if they’re older or had other health problems.
Who’s Most at Risk?
Not everyone is equally vulnerable:
- Age 60+
- Pre-existing lung disease (COPD, asthma)
- Long-term use of high-risk drugs
- History of radiation to the chest
- Smokers
Women are slightly more likely than men to develop methotrexate-induced fibrosis. Nitrofurantoin affects older adults more-often those on daily antibiotics for recurrent UTIs. Amiodarone users need regular lung checks after 6 months of use.
What Should You Do Now?
If you’re taking one of these drugs, don’t panic. But do take action:
- Know your meds. Make a list: prescription, OTC, supplements. Bring it to every appointment.
- Ask your doctor. “Could this drug affect my lungs?” Especially if you’re over 60 or have a history of breathing problems.
- Watch for symptoms. A new dry cough or breathlessness? Don’t wait. Get a chest X-ray or CT scan.
- Don’t stop meds on your own. Abruptly stopping amiodarone or methotrexate can be dangerous. Talk to your doctor first.
Some clinics now do baseline lung function tests before starting high-risk drugs. Ask if it’s an option for you.
The Bigger Picture
More drugs are being approved every year. Many have unknown long-term side effects. Between 2014 and 2024, reports of drug-induced lung damage rose by 23.7%. Regulatory agencies like Medsafe in New Zealand are now pushing for better warnings and mandatory patient education.
But the real gap is in awareness. A 2022 survey found only 58% of primary care doctors routinely ask patients about breathing symptoms when prescribing high-risk drugs. That’s a failure of communication-and it costs lives.
Drug-induced pulmonary fibrosis isn’t a glitch. It’s a known risk. And knowing the signs could save your lungs-or someone else’s.
Can drug-induced pulmonary fibrosis be reversed?
Yes, if caught early. Stopping the drug often leads to improvement within 3 months. But once scar tissue forms, it doesn’t disappear. About 15-25% of patients are left with permanent lung damage, even after treatment. Early detection is everything.
Is nitrofurantoin safe for long-term UTI prevention?
It’s commonly used, but not risk-free. About 1 in 100 long-term users develop lung damage. The risk increases after 6 months of use and is highest in people over 70. Doctors now avoid prescribing it for more than 6 months unless absolutely necessary. Regular check-ups and reporting any new cough or breathlessness are essential.
Do all chemotherapy drugs cause lung damage?
No. Only certain ones-like bleomycin, cyclophosphamide, and methotrexate-have strong links to pulmonary fibrosis. Many chemo drugs don’t affect the lungs at all. Your oncologist should tell you which ones carry this risk. Always ask about lung monitoring if you’re on a high-risk regimen.
Can I take amiodarone if I have mild COPD?
It’s risky. Amiodarone can worsen existing lung disease. If you have COPD or asthma, your doctor should consider alternatives like beta-blockers or calcium channel blockers. If amiodarone is the only option, you’ll need regular lung scans and pulmonary function tests every 3-6 months.
Are there any new drugs that cause pulmonary fibrosis?
Yes. Immune checkpoint inhibitors-used for melanoma, lung cancer, and kidney cancer-are now known to trigger DIPF. These drugs can cause sudden lung inflammation, sometimes within weeks of starting treatment. Doctors now monitor patients on these drugs with chest scans and symptom checks. Newer targeted therapies are also being watched closely for lung side effects.

12 Responses
My grandma was on nitrofurantoin for years for UTIs. She never said a word about coughing until she couldn’t walk to the kitchen without stopping. We thought it was just aging. This post hit hard. I’m going to ask her doctor about a chest scan this week.
I’ve been on methotrexate for psoriasis for 3 years. I’ve had a dry cough since last winter but figured it was allergies. I’m getting a CT scan next week. Thanks for the heads-up - I didn’t realize how common this is.
Let’s be clear: this isn’t just ‘rare side effects.’ This is systemic negligence. Doctors aren’t trained to connect lung symptoms to meds unless it’s obvious. The FDA’s passive reporting system is broken. We need mandatory lung function baselines before prescribing amiodarone, methotrexate, or bleomycin. Period. And patients deserve plain-language warnings - not buried in 40-page inserts.
It’s important to recognize that while the incidence of drug-induced pulmonary fibrosis remains relatively low in absolute terms, the clinical implications are profound, particularly for vulnerable populations such as the elderly and those with preexisting pulmonary conditions. The pharmacokinetic and pharmacodynamic variability among individuals - influenced by genetic polymorphisms in drug-metabolizing enzymes, immune response profiles, and cumulative exposure - renders predictive risk stratification exceedingly difficult. Consequently, heightened clinical vigilance, coupled with patient education and longitudinal monitoring protocols, becomes not merely advisable but ethically imperative. The data presented here underscores a critical gap in post-marketing surveillance and the need for proactive, rather than reactive, pharmacovigilance.
Someone’s gonna die because of this. I know it. I just know it. And no one’s gonna care until it’s too late. My aunt took amiodarone for 18 months, told her cardiologist she was getting winded, and he said ‘you’re old, that’s normal.’ She was 62. She’s on oxygen now. And they still won’t admit it was the drug. This isn’t science - it’s a cover-up.
Thank you for writing this with such clarity and urgency. This is exactly the kind of information that needs to be in every primary care waiting room. I work in a clinic and we’ve had two patients in the last year with undiagnosed DIPF - both were on long-term nitrofurantoin. We’re now implementing a checklist: ‘Any new cough or breathlessness?’ for anyone on high-risk meds. Let’s turn awareness into action.
i just keep thinking… how many of us are walking around with scar tissue in our lungs and think we’re just ‘getting older’? i mean, i had a cough for 6 months after my chemo and thought it was ‘chemo brain’ but for my lungs?? i didn’t even know lungs could get brain fog. i’m gonna go ask my oncologist if my meds could’ve done this. thanks for making me feel less alone about this weird fear.
Amiodarone = lung killer. Don’t ignore cough.
My dad had bleomycin for testicular cancer. He got lung damage after just 3 doses. They didn’t warn us. He’s 75 now and still uses oxygen. I wish we’d known sooner. If you’re on any chemo, ask about lung risks. Don’t wait for symptoms. Ask before you start.
This is an incredibly important post. In India, many patients are prescribed nitrofurantoin for recurrent UTIs without any follow-up. Elderly patients are often not monitored at all. We need awareness campaigns in rural clinics too. I’ve seen cases where patients were misdiagnosed with tuberculosis because no one thought to ask about medications. We need to train doctors to think beyond infections - drug toxicity is real and silent.
my doc just prescribed me methotrexate. i asked if it could mess with my lungs and he said ‘nah, that’s super rare.’ now i’m scared. should i get a baseline scan before starting?
Actually, you’re all missing the bigger point. The real issue isn’t the drugs - it’s that modern medicine treats symptoms, not root causes. Why are people on nitrofurantoin for 10 years? Because we don’t fix the underlying urinary tract anatomy. Why are people on amiodarone? Because we don’t prioritize lifestyle changes first. This isn’t about drug safety - it’s about lazy medicine. Fix the system, not just the warning labels.