What Does It Really Mean to Be a Candidate for a Cochlear Implant?
Many people think cochlear implants are only for those who are completely deaf. That’s not true anymore. If you’re struggling to understand speech even with hearing aids - especially in noisy places like restaurants or family gatherings - you might be a better candidate than you realize. The old rule was clear: wait until you can’t hear anything at all. But today’s guidelines, updated in 2023 by the American Cochlear Implant Alliance, say something very different: don’t wait.
It’s not about how loud things are. It’s about how clearly you understand them. A person with moderate hearing loss who only gets 30% of words right in quiet rooms might benefit more from a cochlear implant than someone with profound loss who still picks up 60% of speech with hearing aids. The key metric? Sentence recognition. If you’re understanding fewer than 50% of words while wearing properly fitted hearing aids, it’s time to get evaluated.
The New Rules: How Candidacy Has Changed Since 2023
Before 2023, most insurance companies and clinics used outdated FDA criteria: you needed a pure-tone average of 70 dB HL or worse at 500, 1000, and 2000 Hz, plus sentence recognition below 40% in your best-aided ear. That excluded a lot of people who were struggling - especially those with asymmetric hearing loss or single-sided deafness.
The 2023 guidelines changed everything. Now, the focus is on functional hearing, not just numbers on an audiogram. The new standard is called the “60/60 rule”: if your better ear has a pure-tone average of 60 dB HL or worse and your word recognition score is 60% or lower with hearing aids, you’re a candidate. Even better - you don’t need to meet both numbers perfectly. If your hearing is a bit better but your speech understanding is terrible, you still qualify.
This shift matters because it catches people who’ve been told, “You still hear well enough.” That’s often the exact moment neural degeneration starts. The brain begins to forget how to process sound. The earlier you intervene, the better the outcome.
What the Evaluation Process Actually Looks Like
Getting evaluated isn’t a single appointment. It’s a full assessment that usually takes 4 to 6 hours spread over two or three visits. First, your hearing aids are checked. Not just turned on - but verified with real-ear measurements to make sure they’re delivering sound correctly. Many people are turned away because their hearing aids aren’t programmed right. That’s not their fault. It’s a system failure.
Then comes the speech testing. You’ll listen to words and sentences - like “cat,” “dog,” “The boy ran to the store” - in quiet and in background noise. The gold standard is the AzBio sentence test. It’s designed to mimic real conversations, not just single words. Your score here tells the team how much your brain is struggling to decode sound.
You’ll also have imaging: a CT scan to check the structure of your cochlea and an MRI to rule out tumors or nerve damage. These aren’t just routine. A malformed cochlea or a damaged auditory nerve can affect whether an implant will work.
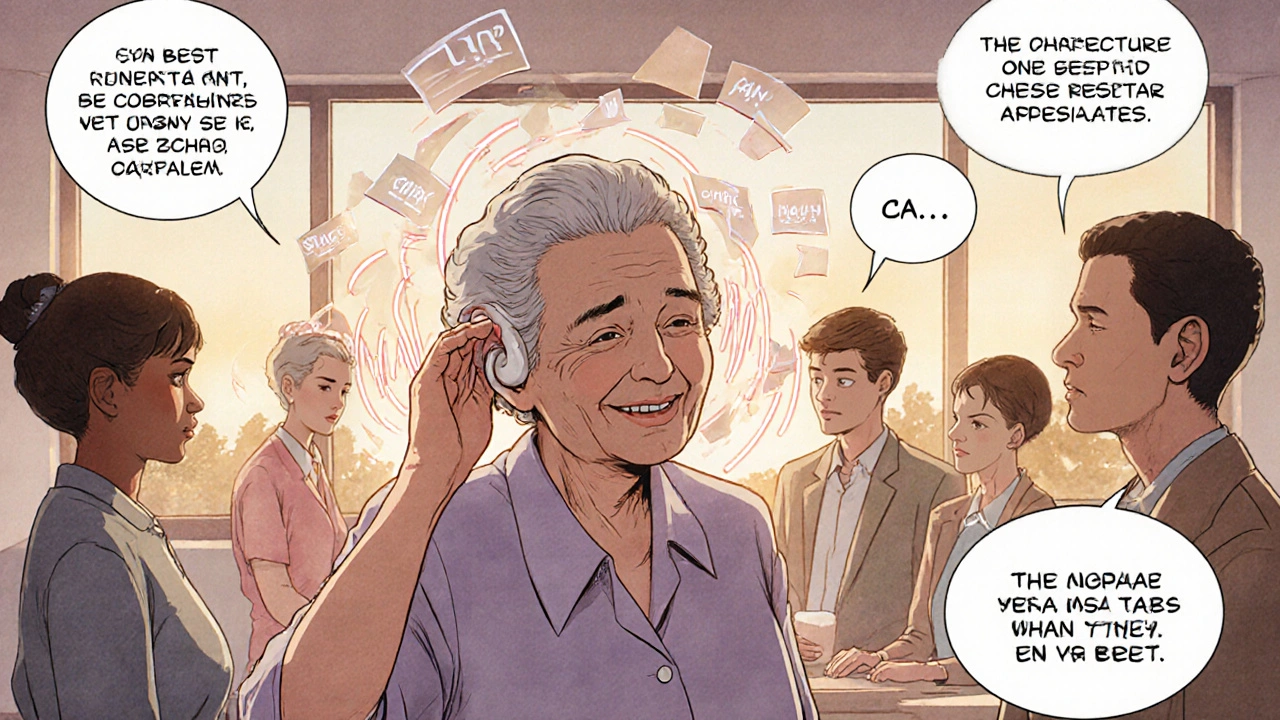
Finally, there’s the human part: a conversation about your goals. Do you want to hear your grandchildren? Talk on the phone? Feel safe walking down the street? Your motivation matters. A cochlear implant isn’t magic. It requires work - listening therapy, adjusting to new sounds, learning to interpret signals your brain hasn’t heard in years.
What Happens After You Get Implanted?
Success isn’t guaranteed - but it’s highly likely if you meet the current criteria. A 2022 study of over 1,200 recipients found that people who qualified under the 60/60 rule improved their sentence recognition by an average of 47 percentage points. That’s not a small gain. It’s the difference between hearing “I’ll be there soon” and hearing nothing at all.
Most people report dramatic improvements in daily life. Ninety-two percent say phone conversations became possible. Eighty-seven percent say listening fatigue - that exhausting mental strain of trying to catch every word - dropped significantly. One woman in her 70s told her audiologist, “I didn’t realize how much I missed the sound of my husband’s laugh until I heard it again.”
But there are limits. Music still sounds robotic for many. Background noise remains challenging, though better than before. Some people need years of therapy to get used to the new sound. The brain adapts slowly. Patience is part of the process.
Why So Few People Get Cochlear Implants - Even When They Should
There are 38 million American adults with disabling hearing loss. Only 128,000 cochlear implants were done in 2022. That’s less than 1%.
Why? Three big reasons:
- Doctors don’t know the criteria. A 2021 JAMA survey found only 32% of primary care physicians could correctly identify when to refer someone for a CI evaluation.
- People think it’s too late. Many believe if they’ve had hearing loss for 10, 15, or 20 years, it’s too late. Research shows that’s false. Outcomes are just as good for long-term users - if their cognitive health is intact and they’re willing to do rehabilitation.
- They’re told to wait. “Try hearing aids longer.” “Wait until you can’t hear at all.” That advice is outdated and harmful.
There’s also a financial myth. Cochlear implants cost $30,000 to $50,000 out of pocket. But Medicare and most private insurers cover them for eligible candidates. And the return on investment? Studies show for every dollar spent on a cochlear implant, society gains $3 in reduced healthcare costs, fewer falls, less dementia risk, and higher employment rates.
Who Still Might Not Be a Candidate?
Not everyone with hearing loss benefits. People with active middle ear infections, severe cognitive decline, or no functional auditory nerve are generally not candidates. Some with profound hearing loss but no desire to engage in rehabilitation may not see improvement - not because the device doesn’t work, but because they don’t use it consistently.
Also, if your hearing loss is caused by something reversible - like a tumor, fluid buildup, or medication side effect - you’ll need to treat that first. Cochlear implants don’t fix the root cause. They bypass it.
And yes - if you’re happy with your hearing aids and understand speech well enough to live your life, you don’t need one. The goal isn’t to implant everyone. It’s to help those who are struggling despite best efforts.

What’s Next? The Future of Hearing Restoration
Research is moving fast. Scientists at Johns Hopkins are testing brainwave responses to sound (cortical auditory evoked potentials) to predict implant success before surgery. Electrocochleography - measuring electrical activity in the inner ear - is also showing promise. These tools could one day replace subjective speech tests with objective data.
By 2030, experts predict cochlear implants will be considered standard care for anyone with bilateral hearing loss over 55 dB HL and speech recognition below 60% with hearing aids. That could expand the eligible population from 1.2 million to nearly 8 million people.
But progress won’t mean anything if disparities continue. In 2022, only 18% of CI recipients were from minority groups - even though those groups make up 40% of people with hearing loss. Access, awareness, and cultural trust are still major barriers.
What Should You Do If You Think You Might Qualify?
If you’re over 50 and find yourself saying “What?” more than you’d like - or if you’re avoiding social events because listening is too hard - don’t wait. Ask your audiologist for a cochlear implant evaluation. You don’t need a doctor’s referral in most cases. Many hearing centers offer free screenings.
Bring your hearing aids. Ask them to verify the fit with real-ear measurements. Request AzBio sentence testing in quiet and noise. Don’t accept “you’re not bad enough yet.” The new guidelines say: if you’re dissatisfied with your hearing aids, you deserve an evaluation.
There’s no downside. Even if you’re not a candidate, you’ll get a baseline of your hearing health - something you can track over time. And if you are? You might get back the conversations, the laughter, the quiet moments you thought you’d lost forever.
Can you still get a cochlear implant if you have some natural hearing left?
Yes. In fact, many people with residual low-frequency hearing are ideal candidates for hybrid or electro-acoustic stimulation implants. These devices combine a cochlear implant with a hearing aid in the same ear, preserving natural hearing while adding electrical stimulation for high frequencies. The 2023 guidelines specifically encourage evaluating each ear individually - even if one ear has better hearing than the other.
Is there an age limit for cochlear implants?
No. There’s no upper age limit. People in their 80s and 90s have successfully received implants and reported major improvements in quality of life. The key factors are overall health, cognitive function, and willingness to participate in rehabilitation - not age. Medicare covers cochlear implants for seniors who meet the criteria.
How long does it take to get results after surgery?
The implant is activated about 2 to 6 weeks after surgery. Initial results are often noticeable within days - sudden clarity in voices, music, or environmental sounds. But full adaptation takes time. Most people see major improvement in speech understanding within 3 to 6 months. Continued progress can happen for up to two years as the brain rewires itself to interpret the new signals.
Do cochlear implants work for single-sided deafness?
Yes. Single-sided deafness (SSD) was not considered a valid indication until the 2023 guidelines. Now, it’s recognized as a major reason for referral. People with SSD struggle with sound localization and understanding speech in noise. Cochlear implants in the deaf ear can restore binaural hearing, improving both spatial awareness and speech understanding by up to 50% in noisy environments.
What if I’ve had hearing loss for 20 years? Is it too late?
No. Long-term deafness doesn’t automatically mean poor outcomes. A 2021 study in Ear and Hearing showed that people implanted after 10+ years of deafness had similar improvements to those implanted sooner - as long as their cognitive abilities were intact and they committed to rehabilitation. The brain can relearn to hear, even after decades. Delaying the implant risks permanent neural degradation, so earlier is better - but it’s never too late to try.
Final Thoughts: Don’t Wait Until It’s Too Late
The biggest mistake people make is waiting. They wait until they can’t hear at all. Until they’re isolated. Until they’ve missed birthdays, phone calls, and conversations with loved ones. The technology has changed. The guidelines have changed. The evidence is clear: if you’re struggling with hearing aids, you’re not failing - the system is failing you.
There’s no shame in asking for help. There’s no penalty for getting evaluated. And if you’re not a candidate? You’ll still walk away with a clearer picture of your hearing health - and peace of mind.
But if you are? You might just get back the sound of your own life.

11 Responses
Let’s be clear: the 2023 guidelines are a bureaucratic overreach. They’re lowering standards under the guise of ‘accessibility.’ If your PTA is 60 dB HL and your word recognition is 60%-you’re not a candidate; you’re a statistic being manipulated to justify device sales. Real hearing loss is when you can’t hear a door slam. Not when you miss a word in a noisy restaurant. This isn’t medicine-it’s industry-driven expansion. The FDA’s old criteria existed for a reason: to prevent over-medicalization of normal age-related decline. Now, every audiologist is a sales rep with a CT scanner.
I just want to say-this article made me cry. Not because I’m hearing impaired, but because I’ve watched my mom go through this. She was told for years, ‘You’re not bad enough.’ She’s 76. She got her implant last year. The first time she heard her cat purr? She sat in silence for ten minutes. Just… listening. I didn’t know a purr could be so loud. Or so beautiful. It’s not about numbers. It’s about moments. The way your grandkid’s voice sounds when they say ‘I love you’ without shouting. The sound of rain on the roof. The quiet joy of not having to ask ‘What?’ five times a minute. Please-if you’re tired of straining, don’t wait. You deserve to hear the world again.
Okay but have you seen the YouTube videos of people hearing for the first time?? 😭 I mean, I’ve watched like 47 of them. The first one I saw-a guy who hadn’t heard his daughter’s voice in 15 years? He just started bawling and said, ‘I forgot what her laugh sounded like.’ Like… how is that not the most powerful thing ever?? I’m not even deaf and I’m crying right now. Also-why is this not on every TV commercial?? Everyone should know this exists. It’s literally magic. And if you’re still using hearing aids and saying ‘I’ll wait’-you’re basically choosing to miss your own life. #CochlearImplantRevolution
Let’s not pretend this is purely about medical progress. It’s also about profit margins. The cochlear implant industry is a $3 billion market. And yes, the guidelines changed because companies lobbied for it. But that doesn’t mean the science is wrong. The data is solid-people do improve. But here’s the uncomfortable truth: we’re not evaluating people’s need. We’re evaluating their willingness to pay for a solution. The real failure isn’t in the audiogram-it’s in the system that makes people wait until they’re isolated, depressed, and desperate before they’re deemed ‘worthy’ of help. The 60/60 rule is a start. But until we fix access, equity, and the stigma around hearing loss, we’re just rearranging deck chairs on the Titanic.
They’re not telling you the truth. The FDA didn’t change the guidelines because of ‘new research.’ They were pressured by the same companies that sell the implants-and those same companies fund the ‘research.’ You think the CT scans and MRIs are for your benefit? They’re to justify the procedure. And what about the brain damage? Once you implant, you’re hooked. You can’t go back. And the ‘rehabilitation’? It’s a 2-year subscription to a corporate wellness program. Don’t believe the hype. This isn’t medicine-it’s a controlled psychological experiment. The real danger? You’ll start believing the noise in your head is gone… when it’s just been replaced with static.
If you’re asking this question, you’re already past the point of ‘maybe.’ Stop waiting. Get evaluated. Now.
-Rebecca
Wow. This is so inspiring! I live in India, and here, hearing loss is still seen as ‘bad luck’ or ‘God’s will.’ No one talks about implants. But I showed this to my uncle-he’s 72, has been hearing poorly for 18 years. He’s going to see an audiologist next week. 🙏 I hope he gets it. I cried reading this. Thank you for writing it. 🌟
Actually, I work in audiology marketing, and I can tell you the 60/60 rule is a marketing win more than a clinical one. We’ve seen a 200% increase in referrals since the guidelines changed-but only 30% of those patients are true candidates. The rest are people who just hate wearing hearing aids. And honestly? Some of them would be better off with better hearing aid fittings or assistive listening devices. But the industry wants volume. So now everyone’s a candidate. And that’s… not always helpful.
I got mine in 2021. Took 14 months to really ‘get’ it. First few months? Everything sounded like a robot singing opera. My wife’s voice? Like a chipmunk on helium. But now? I hear birds. I hear the fridge hum. I hear my daughter whispering ‘I love you’ when she thinks I’m asleep. It’s not perfect. But it’s mine. And I didn’t wait until I was ‘bad enough.’ I waited until I was tired of pretending I could hear. That’s all it took.
India needs this. We have 60 million people with hearing loss. Less than 500 implants per year. Why? Because doctors don’t know. Because families think it’s ‘unnatural.’ Because it’s expensive. But the real problem? Shame. People hide it. They nod along in meetings. They miss birthdays. They pretend. This article should be translated into 10 Indian languages. And posted on every government clinic wall. This isn’t a luxury. It’s a human right.
So let me get this straight-now we’re supposed to implant people who can still hear 60% of words? What’s next? Implanting people who just don’t like their hearing aids? I’ve been in this field 25 years. Back then, we waited until the brain forgot how to hear. Now? We’re implanting people who haven’t even tried a new hearing aid battery. This isn’t progress. It’s desperation dressed up as innovation. And it’s going to backfire. People will get implants, hate the sound, and blame the tech. Then we’ll be back to square one-with even less trust in the system.