Chronic back pain isn’t just a sore back that won’t go away. It’s pain that lasts longer than 12 weeks - long after any injury should have healed. About 8% of adults in the U.S. live with it, and if you’re one of them, you’ve probably tried everything: heating pads, over-the-counter pills, rest, even stretching videos on YouTube. But what actually works? And more importantly, what works long-term without making things worse?
Physical Therapy Isn’t Just Stretching - It’s Rebuilding Your Body’s Mechanics
Physical therapy for chronic back pain isn’t about one magic exercise. It’s about fixing how your body moves. Most people with chronic back pain have developed bad habits - slouching at the desk, favoring one side when walking, holding their breath when lifting. These aren’t laziness. They’re survival tactics your body learned to avoid pain. But over time, they make the pain worse. A good physical therapist starts by figuring out what kind of back pain you have. Is it mechanical? Inflammatory? Nerve-related? That changes everything. For mechanical pain - the kind that flares up with movement - the focus is on core strength. Not crunches. Not sit-ups. The deep muscles that stabilize your spine: the transverse abdominis and multifidus. These muscles don’t show up in the mirror, but they’re the real heroes. Weak? Your spine gets overloaded. Strong? Your back feels lighter. Therapy also includes posture retraining. Not just “sit up straight.” Real, daily practice: how to stand while washing dishes, how to get out of a chair without twisting, how to lift groceries without arching your lower back. Small changes, repeated over weeks, rewire your nervous system. And yes, there’s exercise. But it’s not about pushing through pain. It’s about building tolerance. Studies show people who stick with a consistent home program - even just 15 minutes a day - see 45-55% improvement in function. Those who skip it? Only 45% improvement. The difference isn’t the therapist. It’s consistency.Medications: What Works, What Doesn’t, and What to Watch Out For
Medications are often the first thing people reach for. And for good reason: they can give quick relief. But they’re not a cure. And many come with hidden costs. First-line options are NSAIDs - ibuprofen, naproxen. They reduce inflammation and can cut pain by 30-40% for about 65% of users. But take them for more than a few weeks? Risk of stomach ulcers, kidney strain, even heart problems. The FDA added stronger warnings in 2023. If you’re over 60 or on blood thinners, talk to your doctor before starting. If NSAIDs don’t cut it or cause side effects, doctors often turn to nerve-targeting meds like gabapentin or duloxetine. Gabapentin helps with burning, tingling pain - common in nerve compression. But it can make you feel foggy, dizzy, or tired. One user on Reddit said they had to switch from 900mg of gabapentin to duloxetine because the brain fog made driving dangerous. Duloxetine, an SNRI originally used for depression, works for chronic back pain in about 45% of people. It doesn’t just dull pain - it changes how your brain processes it. Side effects? Nausea in 25%, dizziness in 15%. Most people tolerate it better than gabapentin, but it takes 2-4 weeks to kick in. Opioids? They’re almost never recommended anymore. The CDC reports opioid prescriptions for back pain dropped from 45% in 2016 to just 12% in 2024. Why? Because they don’t fix the problem - they just mask it. Worse, long-term use can cause opioid-induced hyperalgesia: your body becomes more sensitive to pain. You end up needing more pills for less relief. That’s not treatment. That’s a trap.Self-Management: The Real Game-Changer
The most powerful tool you have isn’t a pill or a therapist. It’s you. Self-management means taking control of your daily habits to reduce pain triggers and build resilience. Harvard Health and UCSF both point to structured self-management programs as the key to lasting results. These aren’t apps with cute animations. They’re practical, daily actions:- 20-30 minutes a day of movement - walking, swimming, cycling. Not to burn calories. To flood your spine with blood and oxygen.
- Tracking pain triggers. What makes it worse? Sitting too long? Stress? Poor sleep? Write it down. Patterns emerge.
- Sleep hygiene. Chronic pain disrupts sleep. Poor sleep worsens pain. Break the cycle: cool room, no screens after 9 p.m., consistent bedtime.
- Stress management. Your nervous system stays on high alert with chronic pain. Breathing exercises, mindfulness, even just 5 minutes of quiet each morning can reset your system.
How These Three Work Together - Not Against Each Other
Here’s the truth most people miss: physical therapy, medications, and self-management aren’t options. They’re teammates. Think of it like this: physical therapy fixes the mechanics. Medications reduce the noise so you can move without fear. Self-management keeps everything running long-term. A 2024 study from the Orthopedic Institute of Pennsylvania found that 78% of patients improved significantly with physical therapy alone. But when they added self-management? Improvement jumped to 89%. Add the right medication for nerve pain? It climbed to 92%. The opposite is also true. If you take pills but skip movement, your muscles weaken. If you go to therapy but don’t change how you sit at work, you’re wasting your time. If you do everything but ignore sleep and stress? Pain comes back. The best outcomes happen when all three are used together - not as a last resort, but as a plan from day one.What Doesn’t Work (And Why People Get Frustrated)
Let’s talk about the gaps. Many people quit because they don’t see quick results. Or they hit roadblocks. Insurance limits are a huge issue. Medicare covers only 20 physical therapy visits a year without special approval. Many private plans cap sessions at 12. That’s not enough for lasting change. Some people pay $85 per session out of pocket. That adds up fast. Medication side effects are another reason people give up. One user on Healthgrades said, “I took naproxen for six months. My pain went down, but my stomach felt like it was on fire. I had to stop.” And then there’s the myth of “one solution.” People think, “If this pill doesn’t fix it, nothing will.” But chronic pain doesn’t work like that. It’s not a broken lightbulb. It’s a whole system out of balance.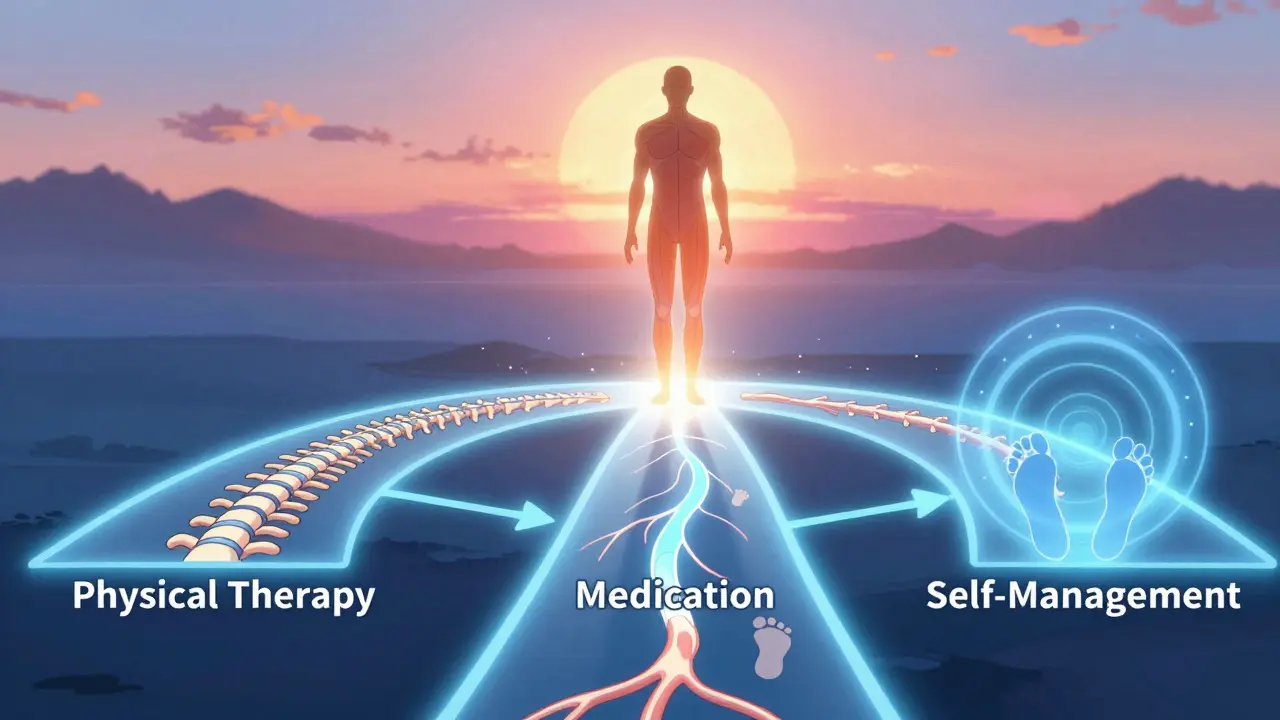
Where to Start - A Simple 30-Day Plan
You don’t need to overhaul your life overnight. Here’s a realistic starting point:- Week 1-2: See a physical therapist for an assessment. Ask them to teach you 2-3 core exercises you can do at home. Do them every morning before coffee.
- Week 3-4: Start a pain journal. Write down your pain level (1-10), what you did the day before, and how you slept. Look for patterns.
- Week 5-6: Add 10 minutes of walking every day. No goal. Just move. If you can’t walk, try seated marches or swimming.
- By Week 8: Talk to your doctor about whether a medication like duloxetine might help - especially if you have burning or tingling pain.
What’s Next? The Future of Back Pain Care
The field is shifting fast. In 2024, the NIH launched a $45 million study to find which patients respond best to which treatments - not based on age or gender, but on biology, movement patterns, and brain activity. This is precision medicine for back pain. Clinics are now using “stepped-care” models: start with therapy and self-management, add medication only if needed, avoid surgery unless absolutely necessary. Employers are catching on too - companies that support these programs see $15,000 in annual productivity gains per employee. The goal isn’t to eliminate pain completely. It’s to make it manageable. To live again. To sleep through the night. To lift your grandkid without fear. That’s possible. Not with one miracle cure. But with a smart, steady plan.Can physical therapy cure chronic back pain?
Physical therapy doesn’t “cure” chronic back pain in the sense of erasing it forever. But it can restore function, reduce pain by 45-55%, and teach your body to move without triggering flare-ups. For many, it’s the most effective long-term solution - especially when paired with self-management.
Are NSAIDs safe for long-term use for back pain?
NSAIDs like ibuprofen and naproxen are safe for short-term use, but long-term use (more than 3-6 months) increases risk of stomach ulcers, kidney damage, and heart problems. The FDA updated warnings in 2023. If you need ongoing relief, talk to your doctor about alternatives like duloxetine or physical therapy.
Why do some people say gabapentin helped but others say it made them foggy?
Gabapentin works best for nerve-related pain - burning, shooting, tingling sensations. But it affects the central nervous system, so side effects like drowsiness, dizziness, and brain fog are common. Dosing matters: starting low (100mg nightly) and increasing slowly reduces side effects. Some people tolerate it well; others don’t. Duloxetine is often a better alternative if brain fog is a problem.
How long does it take to see results from self-management?
Most people start noticing changes in 4-6 weeks with consistent daily effort. Meaningful pain reduction - 40-50% - typically happens after 8-12 weeks. The key is daily practice, not intensity. Even 10 minutes of walking or stretching every day builds up over time.
Is surgery the next step if nothing else works?
Surgery is rarely the first or even second option for chronic back pain. Most cases improve with physical therapy, medication, and self-management. Procedures like spinal cord stimulators or radiofrequency ablation are reserved for severe, refractory cases - and even then, success varies. Only about 50-70% of patients get lasting relief. Always exhaust non-invasive options first.
Can I do physical therapy at home without a therapist?
You can do exercises at home, but you shouldn’t start without a professional assessment. Many people with chronic back pain do the wrong exercises - like too many sit-ups or aggressive stretches - and make things worse. A therapist identifies your specific movement issues and designs a safe plan. After that, home routines are essential for long-term success.


15 Responses
Physical therapy is just another government-funded scam. They want you dependent on them so they can keep billing Medicare. Do push-ups. Lift weights. Stop paying for fancy therapists.
Let me guess - the CDC and FDA are in cahoots with Big Pharma to keep you docile. NSAIDs? They’re just chemical mind control. Gabapentin? That’s the government’s way of making you forget why your spine hurts - because they don’t want you asking questions about why your body’s breaking down. Wake up.
It is imperative to underscore that the tripartite model of intervention - namely, physical rehabilitation, pharmacological adjuncts, and behavioral self-regulation - constitutes the most empirically validated framework for the management of chronic nociceptive dysfunction. The statistical efficacy metrics cited in the source material are robust and align with contemporary clinical guidelines promulgated by the American College of Physicians.
OMG I DID THE 30 DAY PLAN AND MY BACK FEELS LIKE A NEW CAR 😭 I WALKED 10 MINUTES EVERY DAY AND NOW I CAN PICK UP MY KID WITHOUT SCREAMING I LOVE YOU POSTER
It is both regrettable and predictable that the public continues to confuse palliative measures with curative outcomes. The notion that 15 minutes of daily movement constitutes a meaningful therapeutic intervention is not merely naive - it is dangerously misleading. Chronic pain is a neurophysiological cascade, not a lifestyle choice. To suggest that walking or journaling can rewire the central nervous system without addressing underlying biomechanical or biochemical pathology is to engage in pseudoscientific wishful thinking. The data cited, while statistically significant, fails to account for placebo effects, attrition bias, and the absence of long-term follow-up beyond 12 weeks. One must ask: if this were truly effective, why are disability rates for back pain still rising?
There’s something deeply calming about the idea that healing doesn’t require grand gestures. Just consistency. Just showing up for yourself, even when it’s hard. I’ve been doing the 10-minute walk every morning for six months now. Some days I barely move. But I show up. And that’s enough.
...and yet, despite the overwhelming anecdotal evidence, the peer-reviewed literature remains conspicuously silent on the long-term neuroplasticity claims made here... one must question the methodological rigor of studies that rely on self-reported pain scales, especially when the sample populations are self-selected and non-blinded... also, why is no one discussing the role of glyphosate in spinal inflammation?...
bro i tried gabapentin and felt like a zombie 🤪 then i switched to duloxetine and now i can actually sleep 😴 plus i started walking every day and my back feels like it’s got a personal trainer now 🙌 thanks for the real talk
Interesting how everyone treats this like a checklist. You don’t ‘do’ physical therapy. You learn from it. You don’t ‘take’ medication - you trial it. And self-management? That’s not a habit. It’s a relationship with your body. The real failure isn’t the system. It’s expecting one fix to fix everything.
While the article compellingly delineates the synergistic triad of therapeutic modalities, one must consider the confounding variable of socioeconomic stratification: the individual who must work two jobs, lacks transportation to PT sessions, and cannot afford duloxetine (even with insurance) is not merely ‘non-compliant’ - they are structurally disenfranchised. The data is robust, but the applicability is not universal. We must advocate for systemic access, not just individual discipline.
I live in India and we don’t have access to most of this. But I started walking 15 minutes after dinner. No pills. No therapist. Just me and my back. Slowly, it got better. Not perfect. But better. Proof that you don’t need fancy stuff to start healing.
For anyone feeling overwhelmed - start with one thing. One deep breath. One stretch. One minute of standing up. You don’t have to fix everything today. Just be kind to your body. It’s been carrying you through everything. It deserves that.
so like… you’re saying the solution is… not to be in pain? 🤡
Maybe the real question isn’t how to fix the back - but why we keep treating pain like an enemy instead of a messenger. It’s not broken. It’s begging to be heard. And we’ve been shouting over it with pills and push-ups.
My therapist told me to stop trying to ‘fix’ my back and start listening to it. Best advice I ever got. Now I just move how it asks me to. Not how Instagram says I should.