When you start treatment for osteoporosis, waiting a year or two to see if it’s working can feel like gambling with your bones. Bone mineral density (BMD) scans show changes slowly-sometimes not until 12 to 24 months after you begin medication. But what if you could know sooner? That’s where bone turnover markers come in.
What Are Bone Turnover Markers?
Bone is always changing. Old bone breaks down, new bone forms. This process is called remodeling. Bone turnover markers (BTMs) are tiny proteins and fragments released into your blood or urine when bone is being built or broken down. Think of them as real-time signals from your skeleton. There are two main types:- Formation markers: Show new bone being made. Key examples: PINP (procollagen type I N propeptide) and bone alkaline phosphatase.
- Resorption markers: Show old bone being broken down. Key examples: β-CTX-I (beta C-terminal telopeptide of type I collagen) and NTx.
The International Osteoporosis Foundation and other global groups now agree: PINP and β-CTX-I are the best markers to use. They’re accurate, reliable, and respond quickly to treatment.
Why Use Them Instead of Just a DXA Scan?
DXA scans measure bone density. They’re the gold standard for diagnosis. But they’re slow. A 1-3% change in spine density might mean nothing statistically until you’ve been on treatment for over a year. BTMs tell you something different: is your body responding to the drug?Here’s the key difference:
- DXA scan: Tells you how much bone you have.
- BTMs: Tell you what your bones are doing right now.
For example, if you start a bisphosphonate like alendronate, your β-CTX-I levels can drop by 30-50% within just 3 months. That’s a clear sign the drug is working. If your levels stay the same? Something’s off-maybe you’re not taking the pills, or your body isn’t responding.
Studies show patients who hit a 30% drop in β-CTX-I within 3 months have a 1.6% lower risk of fracture after 22 weeks compared to those who don’t. That’s not just a lab number-it’s a real reduction in broken bones.
How Do You Know If the Treatment Is Working?
It’s not enough to just measure BTMs once. You need a baseline and a follow-up.Here’s the standard protocol:
- Before treatment: Get a baseline test. This tells you your starting level.
- 3 months after starting: Test again. This is when you’ll see the clearest change.
- Compare the numbers: For antiresorptive drugs (like bisphosphonates or denosumab), a drop of more than 30% in β-CTX-I or 35% in PINP means you’re responding. For anabolic drugs (like teriparatide), PINP should rise by 70-100%.
The least significant change (LSC)-the smallest real change you can trust-is 20% for PINP and 25% for β-CTX-I. Anything smaller might just be noise.
Non-responders? That’s when BTMs become lifesavers. If your levels don’t move after 3 months, your doctor can switch your drug, check your adherence, or look for other causes-like vitamin D deficiency or kidney problems-before you waste another year on a drug that isn’t working.

What Makes These Tests So Tricky?
BTMs are powerful, but they’re not foolproof. They’re sensitive to small changes in how and when you get tested.Here’s what can throw off your results:
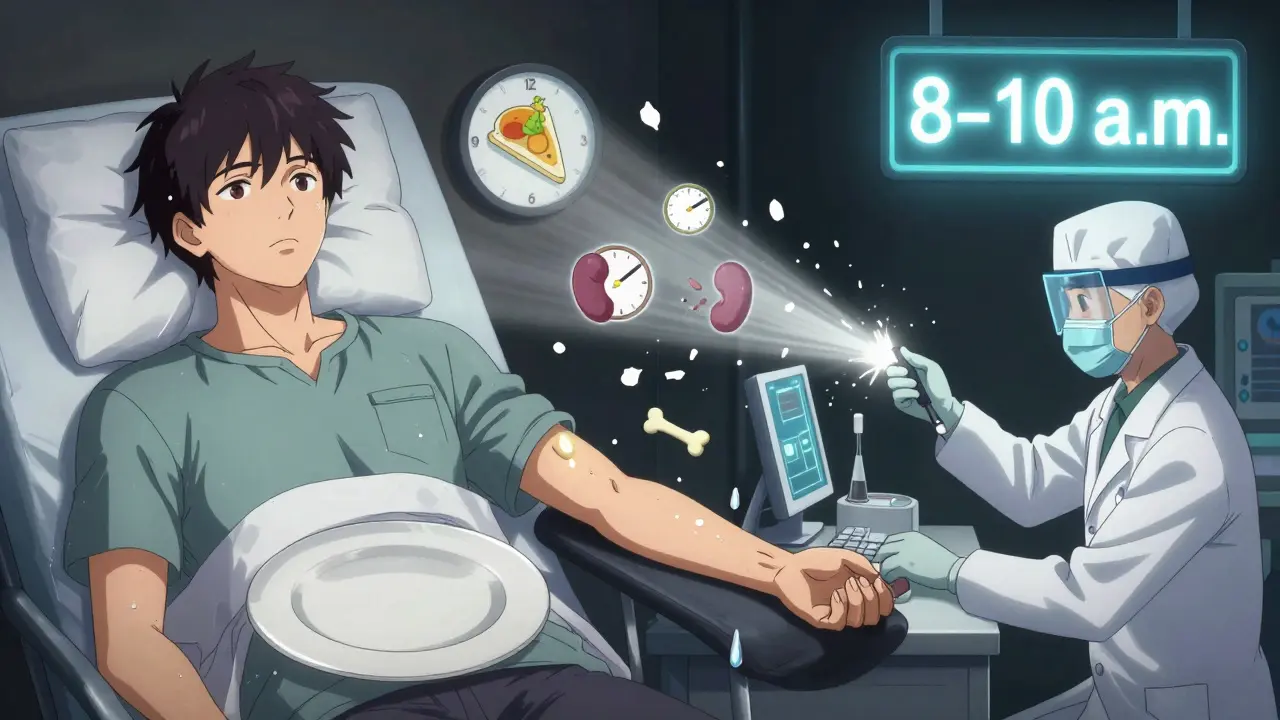
- Food: β-CTX-I jumps 20-30% after eating. You must fast overnight.
- Time of day: CTX levels are highest in the early morning and drop by up to 40% by evening. Samples must be taken between 8 and 10 a.m.
- Menstrual cycle: In premenopausal women, levels fluctuate. Testing should be done in the follicular phase.
- Kidney disease: If you have CKD, your body can’t clear these markers normally. PINP and β-CTX-I may be falsely high. In those cases, bone alkaline phosphatase (BALP) or TRACP5b are better choices.
Even the lab matters. Not all tests are created equal. The assays used must be standardized. As of 2023, only about 65% of U.S. labs follow the recommended IFCC protocols. Ask your doctor which test they’re using.
Who Benefits Most From BTM Testing?
Not everyone needs this. But these groups get the most value:- Patients starting anabolic therapy: Teriparatide or romosozumab cause big, fast changes in PINP. Tracking it confirms the drug is activating bone building.
- Patients with poor adherence: If someone’s skipping pills, BTMs won’t drop. It’s an objective way to spot non-compliance without confrontation.
- Patients with high fracture risk: If you’ve had a fracture on treatment, BTMs can tell you whether the drug failed or if something else is going on.
- People with kidney disease: As mentioned, standard markers don’t work well here. Alternative markers like BALP are essential.
For most healthy postmenopausal women on standard bisphosphonate therapy, BTMs aren’t always needed. But for complex cases, they’re indispensable.
How Do BTMs Fit Into the Bigger Picture?
BTMs don’t replace DXA scans. They complement them.Here’s the ideal monitoring plan:
- At diagnosis: DXA scan + baseline BTM (PINP and β-CTX-I).
- 3 months after starting: Repeat BTM. No DXA yet.
- 12-24 months after starting: Repeat DXA scan. Consider a second BTM if treatment is unclear.
This approach saves time, money, and-most importantly-prevents fractures. One study found BTM-guided monitoring could save $1,200-$1,800 per patient per year by avoiding unnecessary drugs in non-responders.
What’s Next for Bone Turnover Markers?
The field is evolving fast. New research is looking at whether BTMs can predict fracture risk better than BMD alone. Trials are underway to see if adjusting treatment based on BTM levels leads to fewer fractures.Point-of-care tests are in development-imagine getting your BTM result in your doctor’s office the same day. And labs are working on population-specific reference ranges. Right now, most norms are based on Caucasian populations. Asian women, for example, naturally have 15-20% lower β-CTX-I levels. Using the wrong reference range could lead to misdiagnosis.
Medicare in the U.S. has covered PINP and β-CTX-I testing since 2020. Insurance coverage is slowly expanding. The American Association of Clinical Endocrinologists is expected to update its guidelines in 2024 to include formal BTM recommendations.
The message from experts is clear: Bone turnover markers are no longer experimental. They’re a practical, evidence-backed tool for managing osteoporosis. When used correctly, they turn guesswork into confidence.
What If Your BTM Results Are Weird?
Don’t panic. A single odd result doesn’t mean your treatment failed. Here’s what to check:- Did you fast before the test?
- Was the blood drawn between 8-10 a.m.?
- Did you take your osteoporosis medication that day? (Some drugs should be held before testing.)
- Are you taking other meds? Steroids, thyroid hormone, or anticonvulsants can affect BTMs.
- Do you have liver or kidney disease?
If everything checks out and your numbers still don’t move, talk to your doctor about switching therapy. Sometimes, it’s not about compliance-it’s about biology. And that’s exactly why BTMs matter.
What are the best bone turnover markers for monitoring osteoporosis treatment?
The two most reliable markers are serum PINP (procollagen type I N propeptide) for bone formation and plasma β-CTX-I (beta C-terminal telopeptide of type I collagen) for bone resorption. These are recommended by the International Osteoporosis Foundation and European Calcified Tissue Society as the reference markers due to their accuracy, consistency, and fast response to treatment.
How soon can you see changes in bone turnover markers after starting treatment?
Significant changes appear within 3 to 6 weeks, with clear results visible by 3 months. This is much faster than DXA scans, which typically require 12 to 24 months to show measurable changes in bone density. Early response to treatment is best assessed at the 3-month mark.
Do I need to fast before a bone turnover marker test?
Yes, especially for β-CTX-I. You must fast overnight (8-12 hours) because eating can raise CTX levels by 20-30%. Blood should be drawn between 8 and 10 a.m. to avoid natural daily fluctuations. PINP is less affected by food but should still be tested in the morning for consistency.
Can bone turnover markers replace bone density scans?
No. DXA scans remain the gold standard for diagnosing osteoporosis and measuring long-term bone density changes. BTMs are used to monitor early treatment response and adherence. They work best together: BTMs tell you if the drug is working now; DXA tells you if your bones are getting stronger over time.
Why might my bone turnover marker results be high even if I’m on treatment?
High levels could mean you’re not taking your medication as prescribed, your body isn’t responding to the drug, or you have another condition like kidney disease, hyperthyroidism, or vitamin D deficiency. In some cases, especially with anabolic drugs like teriparatide, high PINP is expected and indicates the treatment is working. Always discuss results with your doctor in context.


9 Responses
This stuff is wild. I started my meds and felt nothing, then my doctor said to get the blood test and my numbers dropped like I just quit caffeine. I didn’t even know my bones were talking to me.
Now I check my results like a TikTok follower. No joke, I’m obsessed.
Oh please. You think this is science? It’s just fancy lab theater. The pharmaceutical industry paid for half the studies on PINP and β-CTX-I. You’re being sold a $300 blood test so you’ll keep taking pills you don’t need.
DXA scans are the only real thing. Everything else is noise dressed up in white coats.
And don’t even get me started on fasting. Like I’m gonna skip breakfast for a number that might change next month anyway. I’ve got a life.
While the utility of bone turnover markers in clinical practice is undeniably compelling, one must temper enthusiasm with epistemological humility. The biochemical signals captured by PINP and β-CTX-I reflect dynamic physiological processes, yet they remain proxies-not direct measurements-of skeletal integrity.
Moreover, the assumption that numerical change equates to clinical benefit risks reductionism. Human biology resists quantification in binary terms. A 30% drop may be statistically significant, but it does not, in isolation, guarantee fracture prevention.
Thus, BTMs serve not as arbiters of truth, but as instruments of inquiry-valuable, yes, but only when integrated into the broader tapestry of patient history, comorbidities, and lived experience.
Let us not confuse precision with profundity.
Let’s cut through the noise. If you’re on a bisphosphonate and your β-CTX-I doesn’t drop 30% by 3 months, you’re either non-adherent, malabsorbing, or the drug’s just not working for you.
And yes, fasting matters. I’ve seen patients with ‘failed treatment’ who just ate a bagel before their blood draw. The lab results looked like a horror movie.
Also-kidney disease? Don’t use β-CTX-I. Use BALP. It’s not rocket science, but 70% of docs still get it wrong.
And if you’re on teriparatide? Your PINP should be skyrocketing. If it’s not, you’re wasting time and money. Don’t wait a year. Test at 3 months. Change course. That’s how you save bones.
so i got my btms done and my doctor was like oh you’re responding great but i didnt fast and i had coffee before and now im scared i messed it up
is it even worth redoing or am i just overthinking
also why do they make it so complicated like why not just test anytime lol
also my cousin said her results were weird too and she’s on the same med
is that normal
Why are we letting labs and foreign guidelines dictate how we treat American bones? We’ve got the best doctors, the best tech, and now they want us to follow some European protocol just because they wrote a paper?
DXA is American. BTMs are European. We don’t need their numbers. We’ve got our own way.
And if your doctor pushes this test, ask him if he’s getting paid by the lab. I’ve seen it before.
BTMs? Please. They’ve been using these since the 90s and they never told you the truth. The real reason they push PINP and β-CTX-I is because they’re expensive and insurance pays for them.
Also, did you know the reference ranges are based on white women? Asian women, Black women, even Hispanic women? Their numbers are naturally lower. But the labs still use the same scale. That’s not science. That’s discrimination wrapped in a lab coat.
And if your numbers don’t move? Maybe you’re not the problem. Maybe the system is rigged.
They don’t want you to know that.
Here’s what nobody says: BTMs are a psychological tool disguised as a diagnostic one. They make patients feel like they’re doing something, like they’re in control, when really, they’re just handing over more money and more anxiety.
And let’s be honest-how many people even understand what a pro-collagen peptide is? You give someone a number and they panic. Or they get false confidence. Neither is helpful.
The real issue? We treat osteoporosis like a math problem, not a human one. We reduce bones to numbers and forget that people are scared, tired, and just want to walk without breaking a hip.
BTMs don’t fix that. They just make the silence louder.
bro i got my results and my doctor said i need to retest in 3 months but i dont even have time for this
why do i have to wake up early and not eat and then sit in a lab for an hour
its just bones man
can i not just take my pills and hope for the best
also why is everyone on here acting like this is life or death
its not like i have cancer