Blood Pressure Medication Timing Calculator
This tool helps you determine if switching your blood pressure medication to bedtime dosing might reduce your daytime side effects like dizziness, fatigue, or frequent bathroom trips. It's based on clinical evidence from studies like BedMed and OMAN.
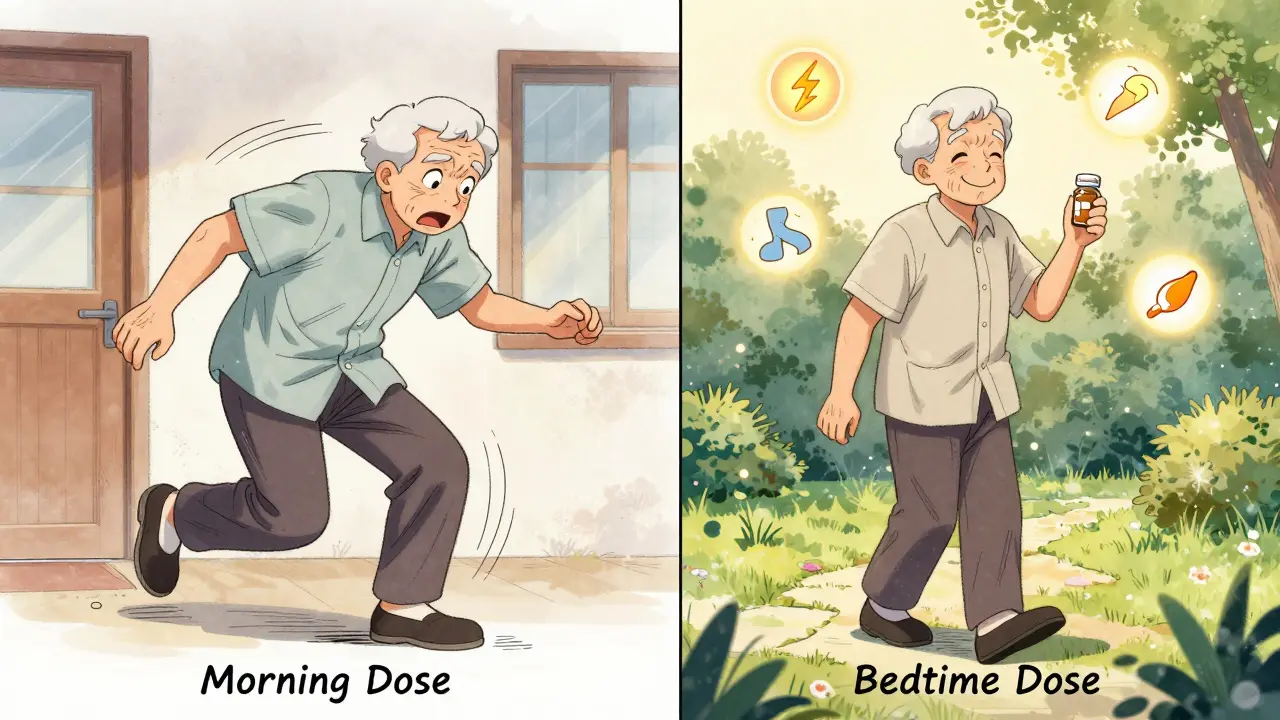
Many people taking blood pressure medication face the same frustrating problem: they feel dizzy, lightheaded, or exhausted right after taking their pill-usually in the morning. This isn’t just inconvenient. It’s dangerous. Dizziness can lead to falls, missed work, or even hospital visits. And when side effects like this happen daily, people stop taking their meds. That’s how high blood pressure becomes a silent killer. The question isn’t just when to take your pill-it’s when to take it so you don’t feel awful during the day.
Why Timing Matters More Than You Think
Your blood pressure doesn’t stay the same all day. It naturally drops at night while you sleep, then rises sharply in the early morning. That’s why heart attacks and strokes are most common between 6 a.m. and noon. Many blood pressure pills are designed to last 24 hours, but if you take them in the morning, the peak effect hits during the day-right when you’re moving around, driving, or working. That’s when dizziness kicks in. Taking the same pill at bedtime shifts that peak to nighttime. Instead of hitting you while you’re trying to make coffee or walk the dog, the medication’s strongest effect happens while you’re lying still. That’s the theory behind bedtime dosing. And it’s not just theory-real data backs it up.What the Research Actually Shows
Large studies like the BedMed trial (over 3,300 patients) and the OMAN trial (720 patients) compared morning vs bedtime dosing over years. The results were mixed on heart attacks and strokes. Some studies showed big benefits with bedtime dosing; others showed no difference. But when researchers looked at side effects, the story changed. In the BedMed trial, patients taking their meds at night reported fewer episodes of dizziness and lightheadedness during the day. The morning group had more of these symptoms-by a noticeable margin. The TIME study found a similar pattern: 24.7% of morning-dosing patients had falls, compared to 22.8% of bedtime-dosing patients. That difference wasn’t statistically significant, but the dizziness numbers were clearer. In the OMAN trial, no extra nighttime risks were found-no dangerous drops in blood pressure while sleeping. That’s important. People worry that lowering blood pressure too much at night could hurt the brain or heart. The data says: not really. One study even looked at bathroom trips, a common side effect of diuretics. Morning dosing led to 40% of patients needing to go during the day. Bedtime dosing dropped that to 36.4%. Not a huge difference, but for someone who works in an office or drives a truck, that 3.6% matters. Less daytime trips mean less stress, fewer interruptions, and more confidence.What About Frail Older Adults?
A special concern is older adults, especially those in nursing homes. They’re more sensitive to blood pressure drops. Could bedtime dosing make them more likely to fall at night? The BedMed-Frail trial looked at exactly this. They tracked falls, fractures, cognitive decline, and confusion. The answer? No difference. Bedtime dosing didn’t increase nighttime risks. It didn’t make people more confused. It didn’t cause more fractures. That’s huge. It means even the most vulnerable patients can safely switch timing-if it helps their daytime symptoms.
Real People, Real Experiences
Clinical trials tell us what happens on average. Real life tells us what happens to you. On Reddit, one user named HypertensionWarrior87 wrote: “Switching my lisinopril to bedtime eliminated the morning dizziness that made me miss work twice last month.” That’s not a statistic. That’s a life changed. But it’s not universal. Another user, SeniorHealth45, said: “Taking amlodipine at night caused such bad leg swelling I had to switch back to morning.” Swelling is a known side effect of calcium channel blockers like amlodipine. For some, it worsens at night. For others, it’s worse in the morning. A survey of over 1,200 patients on MedHelp.org showed that 41% preferred bedtime dosing to avoid daytime bathroom trips. But 29% of them ended up switching back because they were waking up two or three times a night to pee. That’s the trade-off: you might solve one problem, but create another.What Do Doctors Recommend Now?
The American Heart Association says there’s no proven benefit for heart outcomes based on timing. The Joint National Committee says the same. But here’s the catch: they’re talking about heart attacks and strokes. They’re not talking about your ability to get out of bed without feeling like you’re going to pass out. The European Society of Cardiology’s 2024 advice is simple: “Take your pill when you’re least likely to forget.” That’s about adherence. But the Cleveland Clinic and the British Heart Foundation have a more practical rule: “If your first dose makes you dizzy, take it at bedtime until the dizziness goes away.” Then, if you feel fine, you can switch back to morning. A 2024 survey of U.S. doctors found that 43% now talk to patients about timing. Two-thirds of those doctors recommend bedtime dosing specifically to reduce daytime side effects. That’s up from 28% just two years ago.Who Should Try Bedtime Dosing?
You should consider switching to bedtime dosing if:- You feel dizzy, lightheaded, or weak within 2-4 hours after taking your morning pill
- You’re on a diuretic (like hydrochlorothiazide) and need to pee constantly during the day
- You’ve had a fall or near-fall after taking your medication
- You’re on an ACE inhibitor or ARB (like lisinopril, losartan, or olmesartan)
These drugs tend to work better at night and are less likely to cause nighttime low blood pressure. If you’re on a beta-blocker or a calcium channel blocker like amlodipine, the results are less predictable. Talk to your doctor before switching.
Who Should Avoid Bedtime Dosing?
Don’t switch to bedtime if:- You already wake up multiple times at night to urinate (nocturia)
- You have low blood pressure at night (confirmed by home monitoring)
- You’re on a medication that causes leg swelling-some people find it worse at night
- You have sleep apnea or other sleep disorders
If you’re unsure, ask your doctor for a 24-hour ambulatory blood pressure monitor. It tracks your pressure while you sleep and wake. That tells you if your nighttime pressure is already too low.
How to Switch Safely
Don’t just change your pill time on your own. Here’s how to do it right:- Check your current pill label. Some meds are designed to be taken in the morning.
- Call your doctor or pharmacist. Ask: “Is this medication safe to take at night?”
- Start the new timing on a Friday night. That way, if you feel weird, you’re home and can rest.
- Use a blood pressure monitor at home. Take readings at 8 a.m., 8 p.m., and before bed for one week.
- Track symptoms: dizziness, fatigue, swelling, bathroom trips.
- After one week, call your doctor with your log. They’ll tell you if the switch helped-or if you need to go back.
Most people who try this and stick with it report better energy, fewer accidents, and more confidence. That’s not just about blood pressure. It’s about quality of life.
The Bigger Picture
About half of all people with high blood pressure stop taking their meds within a year. The main reason? Side effects. Not high cost. Not complexity. Just feeling awful. Changing the time you take your pill doesn’t cost extra. It doesn’t require new prescriptions. It doesn’t involve surgery. But it can mean the difference between staying on your meds-and living well-and quitting because you feel like garbage every morning. The science isn’t perfect. But the human experience is clear: for many, bedtime dosing reduces daytime suffering. And that’s worth trying.Can I switch my blood pressure pill from morning to bedtime on my own?
No. Always check with your doctor or pharmacist first. Some medications are designed to be taken in the morning, and switching without guidance could cause unsafe drops in blood pressure. Even if your pill seems safe at night, your doctor needs to confirm it’s right for your specific condition and other medications.
Will bedtime dosing cause me to wake up too often at night to use the bathroom?
It might. Diuretics (water pills) are the main culprit. Studies show about 36% of people on bedtime dosing report nighttime urination, compared to 40% during the day. But for some, the switch makes nighttime trips worse. If you already wake up two or more times a night to pee, bedtime dosing may not help. Ask your doctor about a 24-hour blood pressure monitor to check if your pressure drops too low at night.
Does bedtime dosing lower my risk of heart attack or stroke?
The evidence is mixed. Some large studies found a 45-61% drop in heart events with bedtime dosing. Others, like the BedMed trial, found no difference. The American Heart Association says timing doesn’t change your risk of heart attack or stroke. But if bedtime dosing helps you stick to your meds by reducing dizziness or fatigue, you’re more likely to keep your blood pressure under control-which does lower your risk.
What if I forget to take my pill at bedtime?
If you miss your bedtime dose, take it as soon as you remember-unless it’s almost morning. Then skip it and wait until the next night. Don’t double up. Missing one dose won’t cause a spike in pressure. But missing doses regularly does. Set a phone alarm labeled “BP Pill” for 30 minutes before bed. Use a pill organizer with night and day compartments. Consistency matters more than perfect timing.
Are there specific blood pressure meds that work better at night?
Yes. ACE inhibitors (like lisinopril), ARBs (like losartan), and some calcium channel blockers (like amlodipine) tend to have longer-lasting effects and work well with nighttime dosing. Diuretics (like hydrochlorothiazide) can cause nighttime urination, so they’re often better in the morning-unless daytime bathroom trips are worse. Beta-blockers vary. Always ask your doctor which type you’re on and whether timing matters for your specific drug.
How long does it take to notice a difference after switching to bedtime dosing?
Most people notice changes in dizziness or energy within 3-5 days. Blood pressure readings usually stabilize in 7-10 days. Track your symptoms daily. If you feel better, keep going. If you feel worse-like more swelling, confusion, or nighttime urination-call your doctor. Don’t wait a month. Your body responds quickly to timing changes.


15 Responses
i just took my bp med at night and now i cant sleep cause my legs are swelling like balloons?? wtf is this magic??
usa doctors always lie. in india we know blood pressure is a western plot to control the poor. bedtime dosing? more like mind control.
While the clinical data presented is statistically inconclusive regarding cardiovascular outcomes, the behavioral implications of chronotherapy cannot be dismissed on anecdotal grounds alone. The physiological circadian rhythm is a well-documented biological phenomenon, and aligning pharmacokinetics with endogenous rhythms represents a rational, evidence-informed approach to chronic disease management.
we think we’re controlling our bodies with pills, but really the body’s been whispering its rhythm for millennia. morning dosing? that’s the industrial age trying to force a square peg into a round clock. what if the real problem isn’t the medicine-but our refusal to sleep like humans?
bro this is deep. my body been telling me to take my losartan at night since 2021. but doc said 'morning' like its gospel. now i get dizzy at work, feel like i'm in a dream. maybe the system ain't built for us. maybe we gotta rebel with bedtime.
OMG YES!! 🙌 I switched to bedtime and now I actually enjoy my mornings! No more stumbling to the coffee maker like a zombie ☕️💖 #BedtimeDosingIsLife
The paradox of modern pharmacology lies in its precision: we engineer molecules to act upon biological systems, yet we persist in imposing temporal conventions that violate the organism’s intrinsic chronobiology. To administer antihypertensives at dawn is to wage war against the very rhythm that sustains life.
soooo... now i have to remember to take my pill at night? what next? do i have to meditate before bed too?? i just wanna nap after work, not become a health guru 😴
in japan, they take meds after dinner. in mexico, it’s after the siesta. here in the US, we take it when the TV ad says to. we’ve outsourced our biology to pharmaceutical marketing. maybe the real solution isn’t timing… it’s trusting our bodies again.
studies show nothing. big pharma wants you to take it at night so they can sell more monitors and apps. wake up. the pill is just sugar with a label
...I... switched... to... bedtime... and... now... I... can’t... sleep... because... my... brain... is... too... quiet... and... my... blood... pressure... is... too... low... and... I... just... want... to... die... in... peace... 😔
Just switched my hydrochlorothiazide to bedtime last week. Dizziness gone, but I’m up 3x a night now. Still worth it-I’m not falling at work anymore. Use a nightlight, keep a bottle by the bed, and talk to your doc. You got this! 💪
did you know the government put chemicals in the water to make us need meds? now they want us to take them at night so they can track us through our pee? 🤔💧 #DeepStateBP
Respectfully, the clinical evidence remains insufficient to recommend routine timing changes. Individualized assessment is paramount.
Hey Herman, I saw your comment about the night pees. I had the same thing. Then I cut back on fluids after 7pm and it helped a ton. Also, try a pillow under your knees-reduces fluid pooling. Small tweaks, big difference.