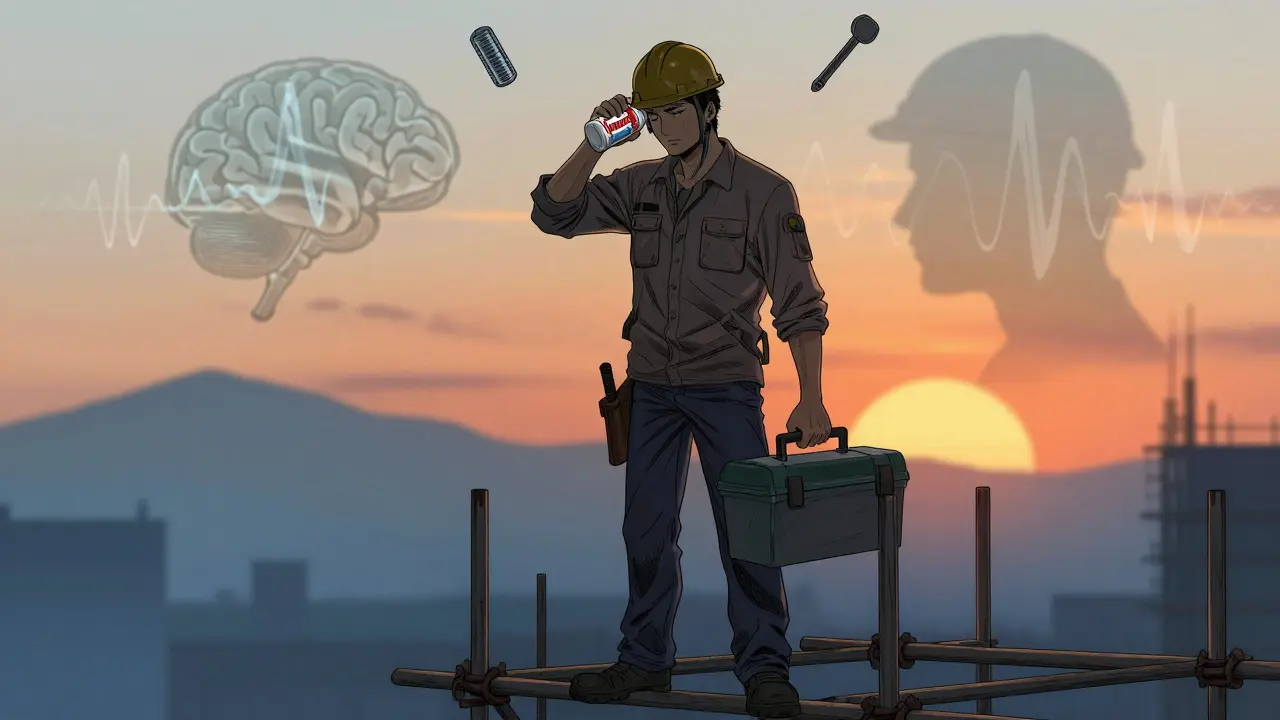
It’s 7 a.m. You’ve been up since 5, juggling a toddler, a deadline, and a stuffy nose from seasonal allergies. You grab a tablet of Benadryl-it’s worked for years. No problem. You’re not sleepy, right? But by 10 a.m., your reaction time slows. You miss a step on the ladder. You nearly rear-end the car in front of you. You don’t feel drunk. You don’t feel tired. But your brain isn’t working like it should.
This isn’t rare. It’s common. And it’s dangerous.
First-generation antihistamines like diphenhydramine, chlorpheniramine, and hydroxyzine are designed to block histamine-chemicals your body releases during allergic reactions. But they don’t stop there. These drugs slip easily through the blood-brain barrier. Once inside, they block histamine in your brain, the very chemical that keeps you alert. The result? Impaired focus, slower reactions, and a dangerous mismatch between how you feel and how you actually perform.
Why You Don’t Feel Drowsy But Still Can’t Work Safely
Here’s the trap: you don’t always feel sleepy. That’s the problem. Studies show people taking first-generation antihistamines often say, "I don’t feel tired," but their performance on cognitive tests drops by 25-30%. In driving simulators, they swerve 50% more than when sober. They miss cues. They freeze. They react too late.
This isn’t just about driving. It’s about operating machinery. Handling sharp tools. Working at heights. Administering medication. Pilots, truck drivers, factory workers, nurses, and construction crews are all at risk. The FAA bans first-generation antihistamines for pilots. The DOT requires employers to consider them in safety protocols. Yet, millions still take them without realizing the risk.
One truck driver on Reddit described failing a roadside cognitive test after taking diphenhydramine. "I didn’t feel sleepy," he wrote. "But I couldn’t touch my nose with my finger. I was awake-just broken inside."
Second-Generation Antihistamines: The Safer Choice
There’s a better option: second-generation antihistamines. These include loratadine (Claritin), cetirizine (Zyrtec), fexofenadine (Allegra), and newer ones like bilastine. They were engineered to avoid the brain.
How? They’re designed to bind to P-glycoprotein transporters-natural pumps in the blood-brain barrier that kick them back out. They don’t cross over. They don’t interfere with brain histamine. That means minimal drowsiness. In clinical trials, their performance is statistically identical to placebo. No impairment. No delay. No risk.
Real-world data backs this up. On Healthgrades, 78% of Allegra users report no drowsiness. Only 12% of Benadryl users say the same. Nurses switching from diphenhydramine to loratadine report better alertness during night shifts. Construction workers say they feel more in control. Even the FDA’s own labeling analysis shows second-generation antihistamines include clearer safety instructions 87% of the time-compared to just 43% for sedating ones.

The Hidden Dangers of First-Generation Antihistamines
It’s not just drowsiness. First-generation antihistamines have a long half-life-up to 30 hours. That means if you take one at 8 p.m., you could still be impaired at noon the next day. Combine that with alcohol, sleep deprivation, or other sedatives, and the risk multiplies.
Autopsy data from aviation accidents shows first-generation antihistamines are the most common medication found in pilots who crashed. The National Highway Traffic Safety Administration estimates 100,000 car crashes each year are linked to drowsiness-and antihistamines are a major contributor. Older adults are especially vulnerable: over a quarter fall each year, and sedating antihistamines increase that risk significantly.
And here’s the kicker: many people don’t even know they’re taking them. Cold and flu mixes, sleep aids, and even some pain relievers contain diphenhydramine or chlorpheniramine. You might think you’re just taking "something for your head," but you’re actually taking a drug that slows your brain.
What Should You Do? A Simple Guide
If you work in a safety-sensitive job-driving, operating machinery, working at heights, handling medical equipment, or even just managing heavy tools-here’s what you need to do:
- Check your labels. Look for diphenhydramine, chlorpheniramine, hydroxyzine, or doxylamine. If you see any of these, put it down.
- Switch to second-generation. Choose loratadine, cetirizine, or fexofenadine. They work just as well for allergies-with no brain fog.
- Test before you work. If you’re trying a new antihistamine, take it at home on a day off. Wait 6 hours. See if you feel slow, fuzzy, or off-balance. Don’t assume you’re fine just because you’re not yawning.
- Wait 24 hours. If you’ve taken a sedating antihistamine, don’t operate heavy machinery or drive until at least 24 hours have passed. The effects linger longer than you think.
- Ask your doctor. If you’re regularly using antihistamines, talk to your doctor about safer alternatives. Most don’t know how common this risk is.

Employers and the Changing Workplace
This isn’t just a personal choice. It’s a workplace issue.
Forty-one percent of Fortune 500 companies now include antihistamine guidance in their occupational health policies. The European Union issued safety alerts for transport workers in 2019. NIOSH launched a 2024 initiative to create formal workplace guidelines. The American College of Occupational and Environmental Medicine predicts that within five years, employers will require safety-sensitive workers to use only non-sedating antihistamines.
Why? Because the cost isn’t just medical-it’s operational. Slower reaction times mean more accidents. More accidents mean more downtime, higher insurance premiums, and lost productivity. One study found that workers on sedating antihistamines were 30% more likely to miss deadlines or make critical errors.
Companies that train employees on this issue see fewer incidents. Simple posters in break rooms. Emails from HR. A quick reminder during safety briefings. These cost nothing-and save lives.
It’s Not About Avoiding Allergy Relief
You don’t have to suffer. You don’t have to choose between breathing and working safely. Second-generation antihistamines are effective, affordable, and widely available over the counter. They’re not new. They’re not experimental. They’re the standard in most developed countries for a reason.
For over 75 years, we’ve been told to reach for Benadryl. But science has moved on. So should we.
Next time your nose is stuffed, don’t grab the first pill you see. Read the label. Ask yourself: "Will this let me do my job safely?" If the answer isn’t a clear yes, don’t take it.
Your brain is your most important tool. Don’t let a cheap antihistamine turn it into a liability.

14 Responses
Bro, I took Benadryl last week for my allergies and thought I was fine… until I tried to pour coffee and spilled it all over my keyboard. Didn’t feel sleepy. Just felt like my brain was wrapped in wet cotton. 🤦♀️
Let me guess-you’re one of those people who thinks America’s getting soft. Back in my day, we worked through anything. If you can’t handle a little drowsiness, maybe you shouldn’t be operating heavy machinery. Or breathing.
Wow. So we’re now policing what people take for allergies? Next they’ll ban caffeine because it makes you jittery. 😒 I work in a hospital and I’ve seen nurses on Zyrtec-zero drama. Meanwhile, the guy on Benadryl? He’s the one nodding off during code blue. Priorities, people.
This is actually really helpful. I didn’t realize my cold medicine had diphenhydramine in it. I’ve been taking it for weeks and wondering why I feel so foggy at work. Switching to Claritin tomorrow. Thanks for the wake-up call 😊
Been on loratadine for years. No drowsiness. No brain fog. Just breathing. Why is this even a conversation anymore?
Good post. Real talk. If you’re in a safety-critical job and you’re still using Benadryl you’re playing Russian roulette with your coworkers. I’ve seen people get hurt because of this. Don’t be the reason someone loses a limb.
YESSSS this needs to go viral!! 🙌 I’m a nurse and I used to take Benadryl for sleep… until I almost gave a patient the wrong med. Switched to Zyrtec and my brain came back. You’re not tired-you’re just broken. Thank you for saying this!! 💪
allergies are a social construct anyway
It’s funny how we’ve normalized chemical impairment in the name of convenience. We don’t let people drive drunk, but we’ll hand out brain-slowing pills like candy. What does that say about our values? 🤔
People who take Benadryl and say they’re fine are the same ones who say "I’m not an alcoholic, I just drink every night." You’re not the exception. You’re the statistic.
i used to take benadryl for my sinuses til i got in a fender bender and the cop asked if i was on anything. i said no. he said you’re acting like you’re high. turns out i was. just with pills. lesson learned.
Oh wow. So now we’re supposed to trust the FDA and pharmaceutical companies? Next you’ll tell me vaccines are safe and the moon landing wasn’t faked. 🙄
THIS IS A GOVERNMENT PLOT. They want us weak. Benadryl is a natural remedy. The FDA banned the truth. They don’t want you to know that your brain fog is a tool for control. The same people who gave you 5G also gave you diphenhydramine. Wake up. 🕵️♀️👁️🗨️
I work in a factory in India. We use chlorpheniramine because it’s cheap. But I’ve seen guys miss shifts, make mistakes. I asked my doctor for alternatives. He said Zyrtec is 2x the price. So I told my boss. Now we’re switching. Small change. Big difference.