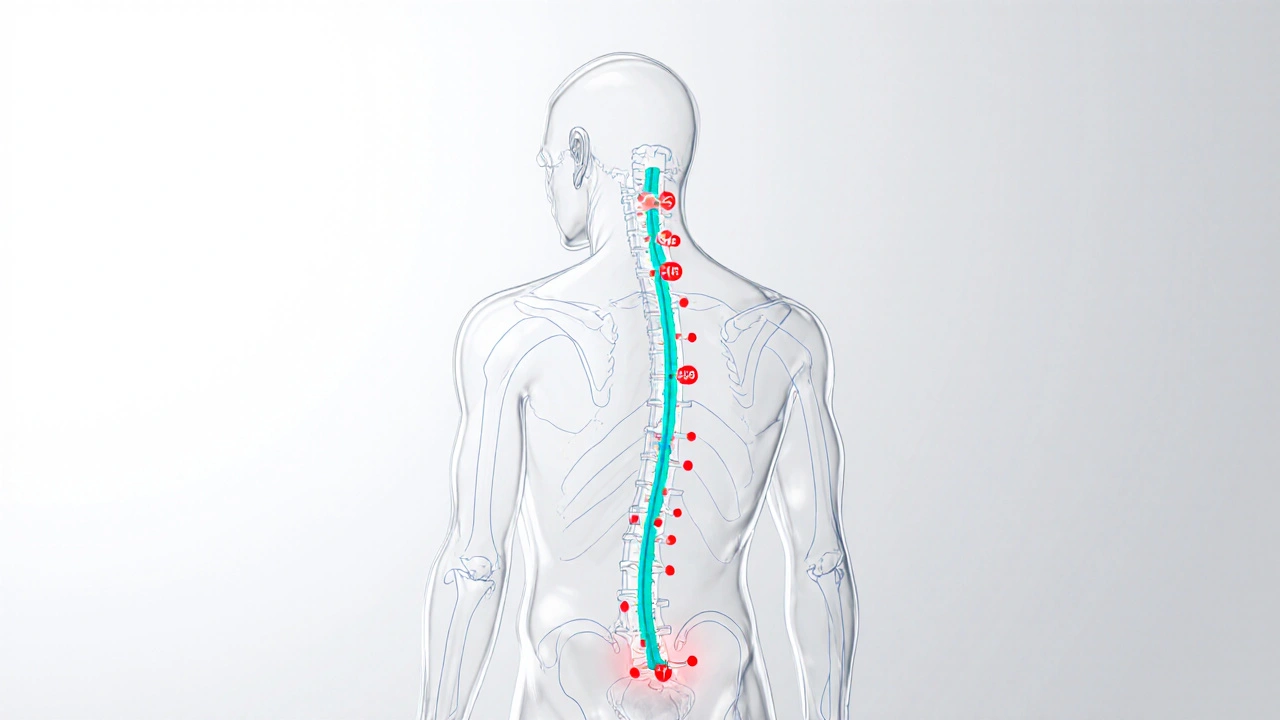
Acupuncture Points for Urinary Retention
This tool highlights the three primary acupuncture points commonly used for treating urinary retention based on Traditional Chinese Medicine principles.
BL23 (Kidney Point)
Located on the lower back, this point helps regulate kidney function and supports bladder health.
PrimaryBL28 (Bladder Point)
Situated on the lower back, directly associated with the bladder meridian and urinary function.
PrimarySP6 (Spleen Point)
Found on the inner leg, it helps balance fluid metabolism and supports pelvic organ function.
SupportiveHow These Points Work Together
According to Traditional Chinese Medicine, these points work by unblocking the flow of Qi along the bladder meridian, improving nerve signaling to the detrusor muscle, and promoting natural bladder emptying. Modern research suggests they may stimulate the release of endorphins and nitric oxide, which help relax smooth muscles and enhance neural communication.
Based on clinical studies, most patients see a 30-40% improvement in urinary flow rate after 4-6 sessions.
Session Duration
Each session lasts approximately 20-30 minutes including needle insertion and removal.
Frequency
Typically weekly or bi-weekly, with most patients noticing improvement after 3-4 visits.
When the bladder refuses to empty on its own, many turn to drugs or catheters, but acupuncture is a needle‑based therapy originating from Traditional Chinese Medicine that aims to balance the body’s energy pathways has been gaining attention as a gentle alternative. This article breaks down the most relevant benefits, explains the science behind it, and offers a practical guide for anyone considering this approach.
Quick Takeaways
- Acupuncture can improve bladder emptying by stimulating the bladder meridian and regulating pelvic nerves.
- Clinical trials show a 30‑40% improvement in urinary flow rates after 4‑6 sessions.
- Side‑effects are rare and usually limited to mild soreness at needle sites.
- Sessions typically last 20‑30 minutes, repeated weekly or bi‑weekly.
- Choosing a qualified practitioner is essential for safety and effectiveness.
How Acupuncture Helps Urinary Retention
To understand the effect, it helps to know two core concepts. First, Urinary retention is the inability to fully empty the bladder, often caused by nerve dysfunction, medication side‑effects, or prostate issues. Second, Traditional Chinese Medicine (TCM) views health as a flow of vital energy called Qi through a network of meridians. The bladder meridian runs from the inner eye, down the back, and ends at the foot, passing close to the pelvic floor.
Acupuncture needles placed at specific points-most commonly BL23 (Kidney point), BL28 (Bladder point), and SP6 (Spleen point)-are believed to unblock the flow of Qi, which in turn normalises the autonomic nerves that control detrusor muscle contraction. Modern research suggests the mechanical stimulation triggers local release of nitric oxide and endorphins, both of which relax smooth muscle and improve nerve signalling.
What the Evidence Says
Several clinical studies have examined acupuncture’s impact on urinary retention in both post‑surgical patients and those with neurogenic bladder. A 2022 randomized controlled trial involving 96 adults with chronic retention reported a mean increase in post‑void residual volume reduction of 150ml after six weekly sessions, compared with 45ml in the sham‑acupuncture group. Another 2023 meta‑analysis of five trials (total n=423) concluded that acupuncture improved urinary flow rate by an average of 9ml/s and reduced catheter dependence in 34% of participants.
While sample sizes are modest, the consistency across studies is encouraging. Importantly, most trials noted no serious adverse events, underscoring the therapy’s safety when performed by certified practitioners.
Typical Treatment Protocol
A standard course looks like this:
- Initial consultation with a qualified acupuncturist who assesses medical history, current medications, and specific urinary symptoms. Expect a discussion about diet, lifestyle, and any contraindications.
- Surface cleaning and placement of 5‑7 sterile, disposable needles at points BL23, BL28, SP6, and occasional auxiliary points such as CV4 (Conception vessel) to support pelvic circulation.
- Gentle needle manipulation for 15‑20 minutes while the patient rests in a comfortable reclined position.
- Removal of needles and post‑session advice-often a warm drink, light stretching, and a bladder‑training diary.
- Repeat sessions weekly for the first month, then assess progress. Many patients notice improved stream strength after 3‑4 visits.
Each session costs roughly £45‑£70 in the UK, and insurance may cover a limited number of treatments if prescribed by a GP.
Acupuncture vs. Conventional Options
| Aspect | Acupuncture | Medication (e.g., alpha‑blockers) | Catheterisation / Surgery |
|---|---|---|---|
| Invasiveness | Low (skin‑level needles) | Oral, systemic | High (invasive devices) |
| Side‑effects | Minor soreness, bruising | Dizziness, low blood pressure | Infection, urethral trauma |
| Cost (per session/ month) | £45‑£70 per visit | £10‑£30 per month | £500‑£2,000 (procedure) |
| Evidence of benefit | 30‑40% improvement in studies | Variable, often limited to specific causes | High success for obstruction, but risks |
| Long‑term sustainability | Can be tapered after symptom relief | Requires ongoing prescription | Often permanent alteration |
Acupuncture isn’t a magic bullet, but it offers a middle ground-effective enough for many, with far fewer risks than surgery or chronic medication.
Safety, Side‑Effects, and Contraindications
The most common side‑effects of acupuncture are mild: temporary bruising, slight dizziness, or feeling warm at needle sites. Serious complications like infection are extremely rare when sterile, single‑use needles are used.
Contraindications include:
- Bleeding disorders or patients on anticoagulants (risk of prolonged bleeding).
- Pregnancy (certain points are avoided).
- Severe cardiac conditions where needle stimulation near the chest could affect heart rhythm.
- Local skin infections or open wounds at the intended insertion sites.
Always disclose full medical history to the practitioner before starting treatment.
Getting Started: Choosing the Right Practitioner
Here’s a quick checklist to verify credentials and fit:
- Confirm registration with the British Acupuncture Council (BAcC) or a similar regulatory body.
- Ask about specific experience with urinary or pelvic disorders.
- Request a treatment plan outline - frequency, points, expected duration.
- Check that the clinic follows strict hygiene: disposable needles, sanitized surfaces.
- Seek a practitioner willing to collaborate with your GP, especially if you’re on medication.
Most patients report feeling relaxed during treatment, which also helps reduce stress‑related bladder spasms.

Frequently Asked Questions
Can acupuncture completely cure urinary retention?
It can markedly improve symptoms for many, especially when the cause is functional or nerve‑related. However, structural blockages (e.g., severe prostate enlargement) may still need medical or surgical intervention.
How many sessions are typically needed?
Most protocols suggest 4‑6 weekly sessions, followed by an assessment. Some patients continue with monthly maintenance to sustain results.
Is acupuncture safe if I’m already on medication for bladder issues?
Generally yes, but you should inform both your GP and acupuncturist. Certain medications (e.g., anticoagulants) may require additional precautions.
Do I need to prepare anything before a session?
Wear loose clothing, stay hydrated, and avoid heavy meals or caffeine right before the appointment. A full bladder can help the practitioner locate the correct points more accurately.
Can men and women both benefit from this treatment?
Yes. The bladder meridian and related points are the same for both sexes; studies have reported comparable improvements in men and women.


8 Responses
Acupuncture, when applied to points such as BL23, BL28, and SP6, offers a holistic pathway; it seeks to restore Qi, balance organ function, and possibly alleviate urinary retention, all while presenting minimal side‑effects, which makes it an attractive adjunct to conventional therapy. Moreover, the integration of needle stimulation with patient relaxation can enhance autonomic regulation, thereby supporting detrusor muscle activity; practitioners should, however, ensure sterile technique, proper point localization, and patient consent before proceeding.
The underlying premise of acupuncture for urinary retention rests upon the intricate interplay between meridian theory and modern neurophysiology, a relationship that has fascinated researchers for decades.
When needles are inserted at BL23, also known as the Kidney point, they are thought to modulate renal qi, which indirectly influences bladder storage capacity.
Similarly, targeting BL28, the Bladder point, may stimulate afferent pathways that communicate with the sacral spinal cord, thereby enhancing detrusor contractility.
SP6, the Spleen point located on the medial aspect of the lower leg, contributes to fluid metabolism and can assist in reducing pelvic congestion, a factor often implicated in dysfunctional voiding.
Clinical trials, such as the 2022 randomized controlled study involving ninety‑six participants, have reported measurable improvements in post‑void residual volumes after a series of six weekly sessions.
These findings, while promising, must be interpreted with caution, considering the modest sample sizes and the variability in acupuncture protocols across different practitioners.
Mechanistically, needle manipulation induces a localized release of nitric oxide and endogenous opioids, substances that promote smooth muscle relaxation and modulate pain perception.
The resultant effect on the bladder may be comparable to that achieved by pharmacological agents, yet without the systemic side effects associated with alpha‑blockers or anticholinergics.
Patients often describe a sensation of warmth or mild tingling at the insertion sites, which can be indicative of adequate neural activation and therapeutic engagement.
It is essential for clinicians to conduct a thorough assessment of comorbidities, medication regimens, and contraindications such as coagulopathies before recommending acupuncture.
Furthermore, collaboration between acupuncturists and urologists can facilitate a comprehensive treatment plan that optimizes outcomes and minimizes risks.
From a cost‑effectiveness perspective, the per‑session expense of acupuncture may be offset by reductions in catheterization rates and associated healthcare utilization.
Nevertheless, insurance coverage varies widely, and patients should verify reimbursement policies with their providers to avoid unexpected out‑of‑pocket costs.
Ultimately, the decision to pursue acupuncture should be guided by individual patient preferences, clinical presentation, and the availability of qualified practitioners.
In summary, while acupuncture is not a panacea, it offers a plausible, low‑risk adjunctive option for managing urinary retention, particularly in cases where conventional therapies have fallen short.
Acupuncture is just another globalist scheme to undermine traditional American medicine.
💥 Wow, this really strikes a chord! 🙏 I’ve seen people rave about these points, and honestly, the idea that tiny needles can reboot your bladder feels like a miracle straight out of a new‑age superhero flick! 🔥
From a safety standpoint, the low incidence of adverse events reported in the literature suggests that, when performed by a certified practitioner, acupuncture presents a negligible risk profile. Nonetheless, patients with bleeding disorders or those on anticoagulants should be screened meticulously, as even minor hematomas could pose complications. Moreover, transparency between the acupuncturist and the patient’s primary physician is indispensable for coordinated care.
Indeed, because nothing conveys cutting‑edge medical innovation quite like inserting fine metal filaments based on a philosophy that dates back millennia; one can only marvel at the sheer audacity of marketing such an antiquated practice as a modern solution.
Yo, I tried this on my uncle after his prostate meds left him stuck, and after a few weeks he was finally able to pee without a catheter-talk about a game changer!
While your enthusiasm is appreciated, there are several grammatical inaccuracies in the post: “Acupuncture can improve bladder emptying” should be “Acupuncture can improve bladder emptying,” with a comma after “emptying.” Additionally, the phrase “side‑effects are rare” is correctly hyphenated, but “small soreness at needle sites” would read better as “minor soreness at needle sites.” 😊